If you have been trying to conceive for any length of time, you have likely realized that the journey often feels less like a romantic endeavor and more like a high-stakes science project. You become an amateur endocrinologist, tracking temperatures, examining charts, and learning a new vocabulary of acronyms. Among all the data points you track—basal body temperature, cervical mucus quality, and progesterone—one stands out as the absolute gatekeeper of conception: the LH surge.
Table of Contents
While estrogen builds the lining of your uterus and progesterone maintains a potential pregnancy, luteinizing hormone (LH) is the spark that lights the fire. It is the biological trigger that sets the actual release of the egg in motion. Without this specific hormonal event, conception is biologically impossible, regardless of how perfect the rest of your cycle appears or how well-timed your intercourse might be.
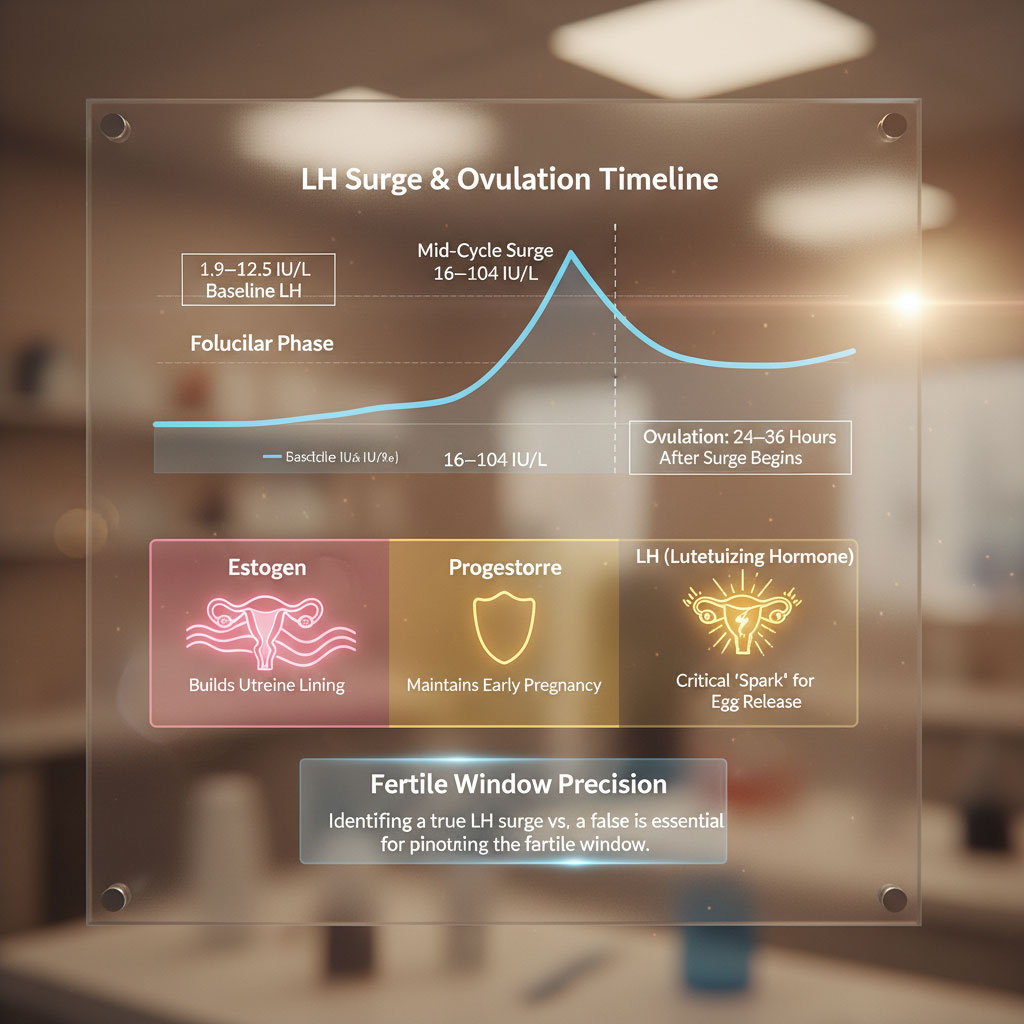
For most women, ovulation typically occurs 24 to 36 hours after this surge begins. In the United States, normal baseline LH levels in the follicular phase (the first half of your cycle) usually range from 1.9 to 12.5 IU/L. However, during the critical mid-cycle peak, those levels must skyrocket, generally spiking between 16 and 104 IU/L. Identifying this specific window—and distinguishing a true surge from a “false start”—is the most effective way to pinpoint your fertile window and maximize your chances of pregnancy.
This comprehensive guide goes beyond the basics. We will explore the clinical specifics of normal LH levels, dissect the complex biological mechanisms behind the surge, provide a masterclass on interpreting test results using US medical standards, and discuss exactly what it means if your numbers fall outside the expected range.
The Biology of the LH Surge: The Trigger for Conception
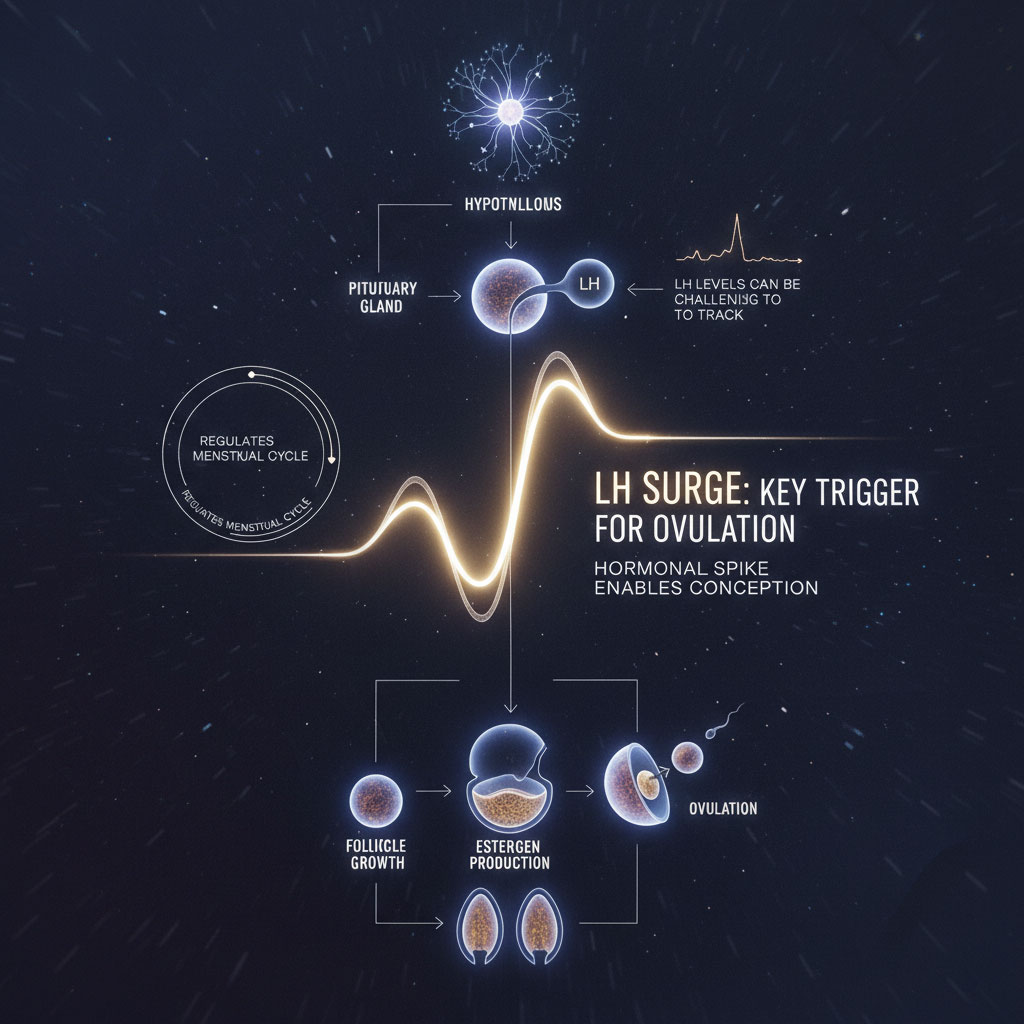
To truly understand why LH hormone levels matter, and why they can sometimes be so tricky to track, we must look beneath the surface at the sophisticated communication system operating within your body. The reproductive system relies on a complex feedback loop known as the Hypothalamic-Pituitary-Ovarian (HPO) axis. This axis acts as a command center, regulating the release of hormones that drive the menstrual cycle.
The “Pulse” of Luteinizing Hormone
Luteinizing hormone (LH) is a gonadotropin produced by the pituitary gland, a pea-sized organ located at the base of the brain. It is important to note that LH is not released in a steady stream like water from a faucet. Instead, it is released in pulses. These pulses are controlled by a hormone called Gonadotropin-Releasing Hormone (GnRH) released by the hypothalamus.
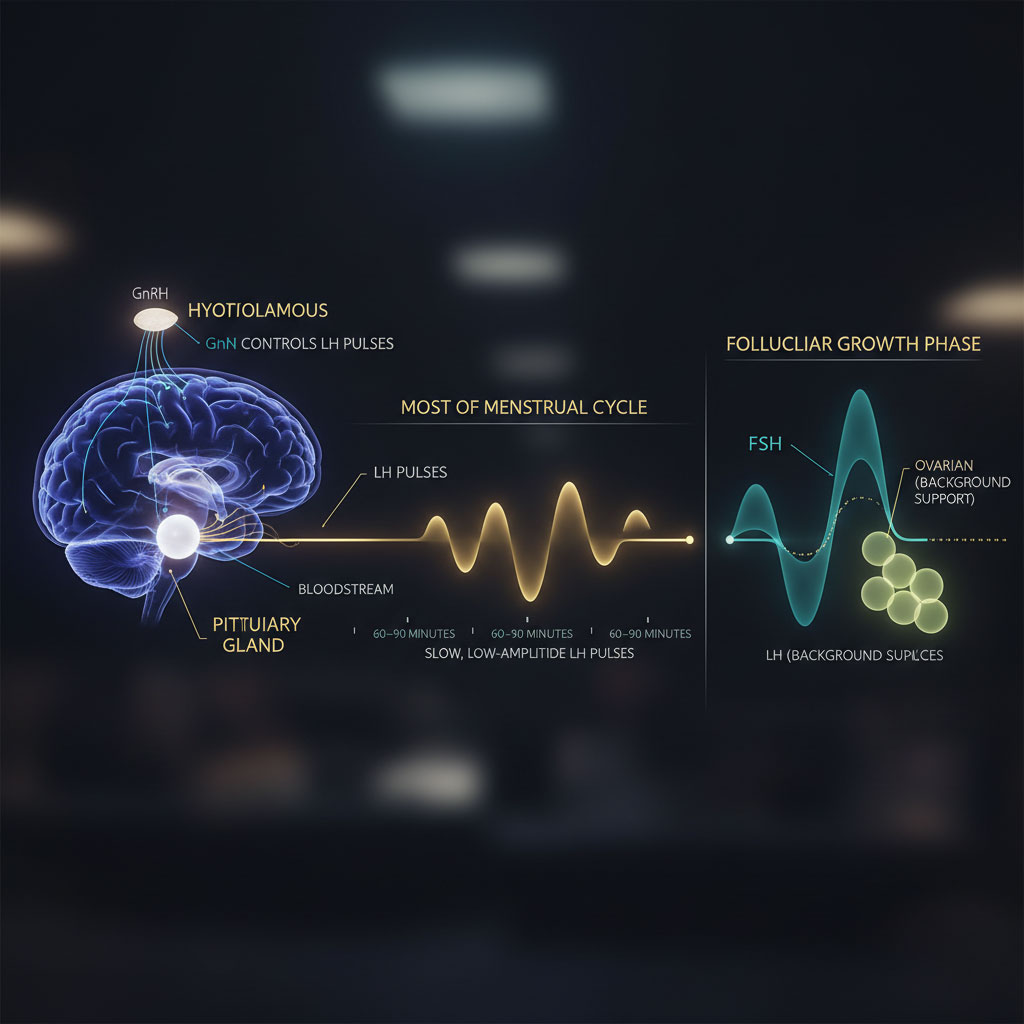
During the majority of your menstrual cycle, these pulses are slow and low-amplitude, occurring roughly every 60 to 90 minutes. LH waits in the background while another hormone, Follicle-Stimulating Hormone (FSH), takes the lead. As its name suggests, FSH encourages the recruitment and growth of ovarian follicles—the fluid-filled sacs that contain your microscopic eggs.
The Estrogen Feedback Loop: The Switch
As these follicles grow during the first half of your cycle (the follicular phase), they produce estrogen (specifically estradiol). This estrogen production is crucial. It acts as a signal to the brain, essentially reporting on the development of the egg.
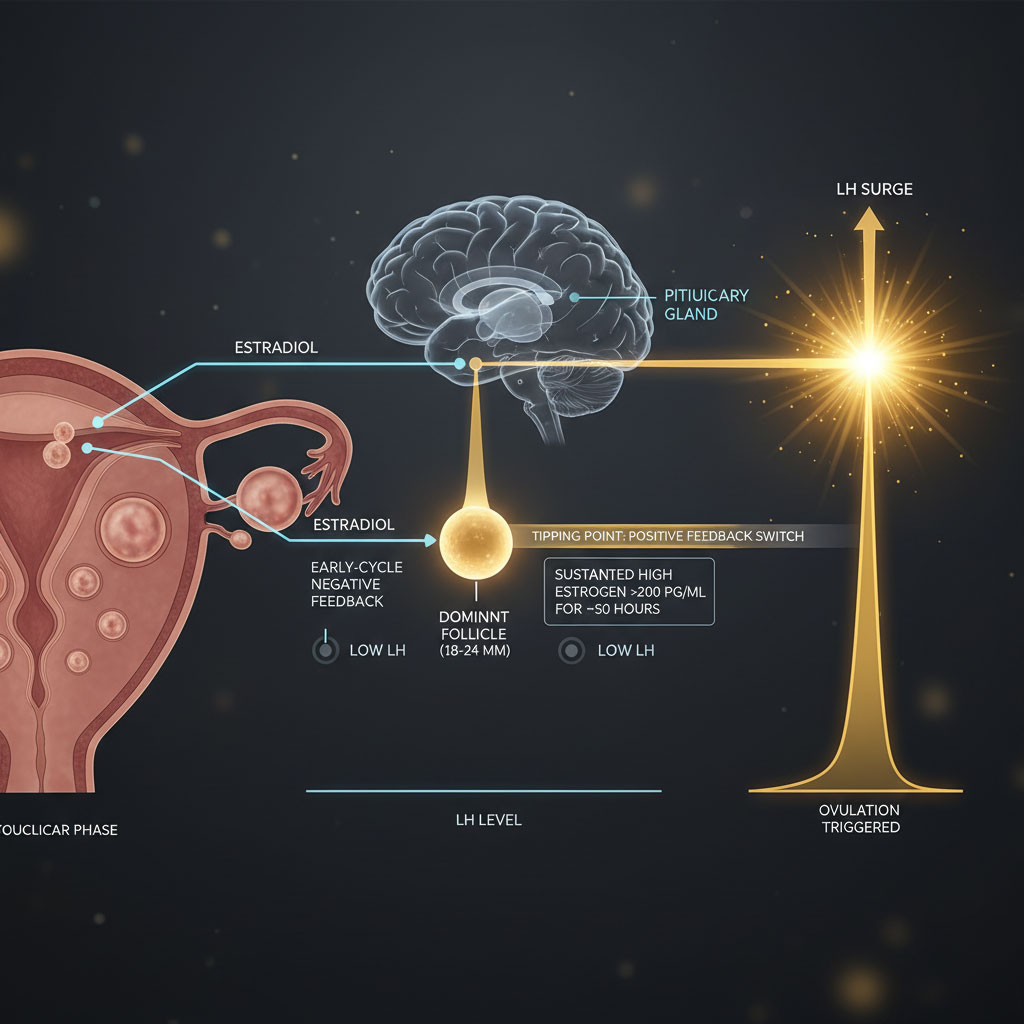
In the early stages of the cycle, estrogen exerts a negative feedback on the brain. It tells the pituitary, “We are growing, keep the LH low.” This prevents premature ovulation of an immature egg. However, biology has a fascinating tipping point. Once a dominant follicle reaches maturity (usually around 18-24mm in size), it pumps out a massive, sustained amount of estrogen. When estrogen levels stay above a certain high threshold (typically >200 pg/mL) for about 50 hours, the feedback loop flips from negative to positive.
This high estrogen level acts as a biological “switch.” It tells the pituitary gland that the egg is fully mature and ready for release. The pituitary responds by dumping its stored reserves of LH into the bloodstream in a massive, sudden burst. This is the surge.
How the Surge Physically Causes Ovulation
This sudden spike is what we call the LH surge. It is not just a chemical signal; it causes a cascade of physical changes within the ovary within hours:
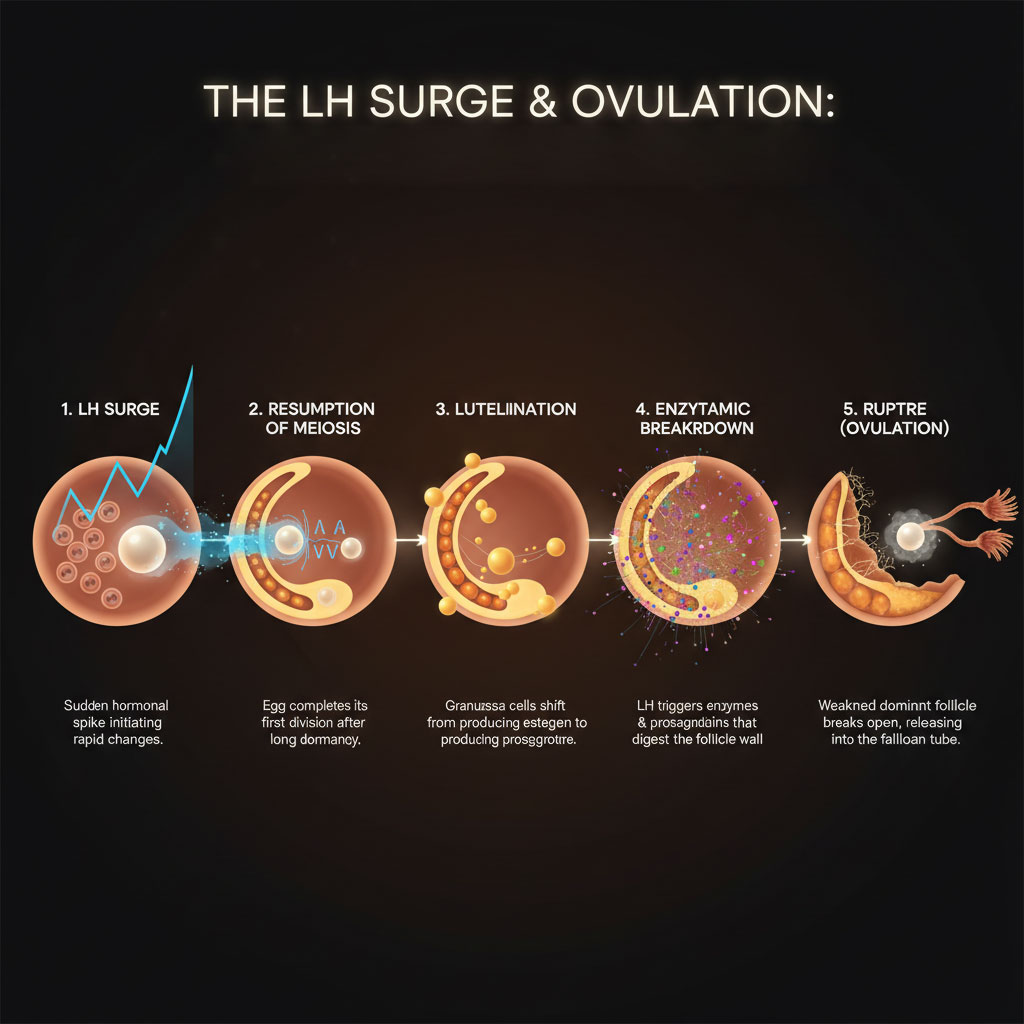
- Resumption of Meiosis: The egg inside the follicle, which has been dormant in a state of suspended animation since you were a fetus, completes its first division and becomes ready for fertilization.
- Luteinization: The cells surrounding the egg (granulosa cells) start changing their chemistry to produce progesterone instead of just estrogen.
- Enzymatic Breakdown: The surge triggers the release of enzymes and inflammatory mediators like prostaglandins) that digest the wall of the follicle.
- Rupture: The wall of the dominant follicle weakens, dissolves, and eventually ruptures. This explosive release of the egg into the fallopian tube is ovulation.
Without this specific surge, the egg remains trapped. This means that even if you have a regular period and shed your lining every month, you might not be ovulating if your LH levels do not spike high enough or long enough to trigger the release. This condition, known as Luteinized Unruptured Follicle (LUF) syndrome or anovulation, is a common cause of unexplained infertility.
The Critical 24-36 Hour Window
Timing is precise here, but it is also a source of confusion. It is vital to understand that the LH surge does not cause immediate ovulation. Instead, it starts a biological countdown clock.
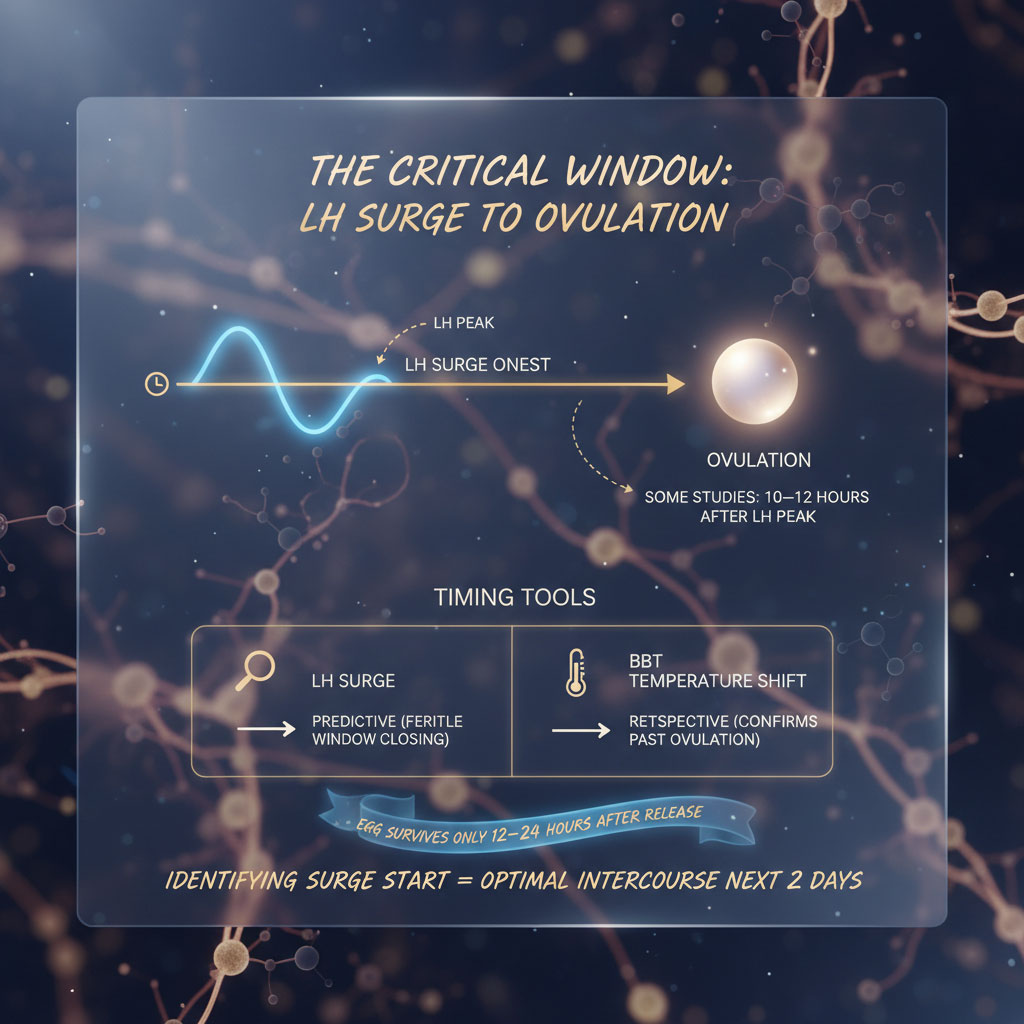
Clinical guidelines indicate that ovulation usually happens 24 to 36 hours after the surge begins (onset). Some detailed studies suggest it occurs about 10 to 12 hours after the LH reaches its absolute peak concentration.
This delay is exactly why identifying the start of the surge is so valuable for conception. It gives you a heads-up that your fertile window is closing and that the next two days are the optimal time for intercourse. If you wait until after you have ovulated to try (for example, waiting for a temperature shift on a BBT chart), the egg may no longer be viable, as it typically survives only 12 to 24 hours after release. Therefore, the LH surge is a predictive tool, whereas temperature is a retrospective tool.
Analyzing Normal LH Levels: The Clinical Guidelines
When you receive lab results from a fertility clinic or use a quantitative ovulation test at home, you will often see numbers measured in IU/L (International Units per Liter) or mIU/mL (milli-International Units per milliliter)—these units are generally treated as equivalent in fertility testing.
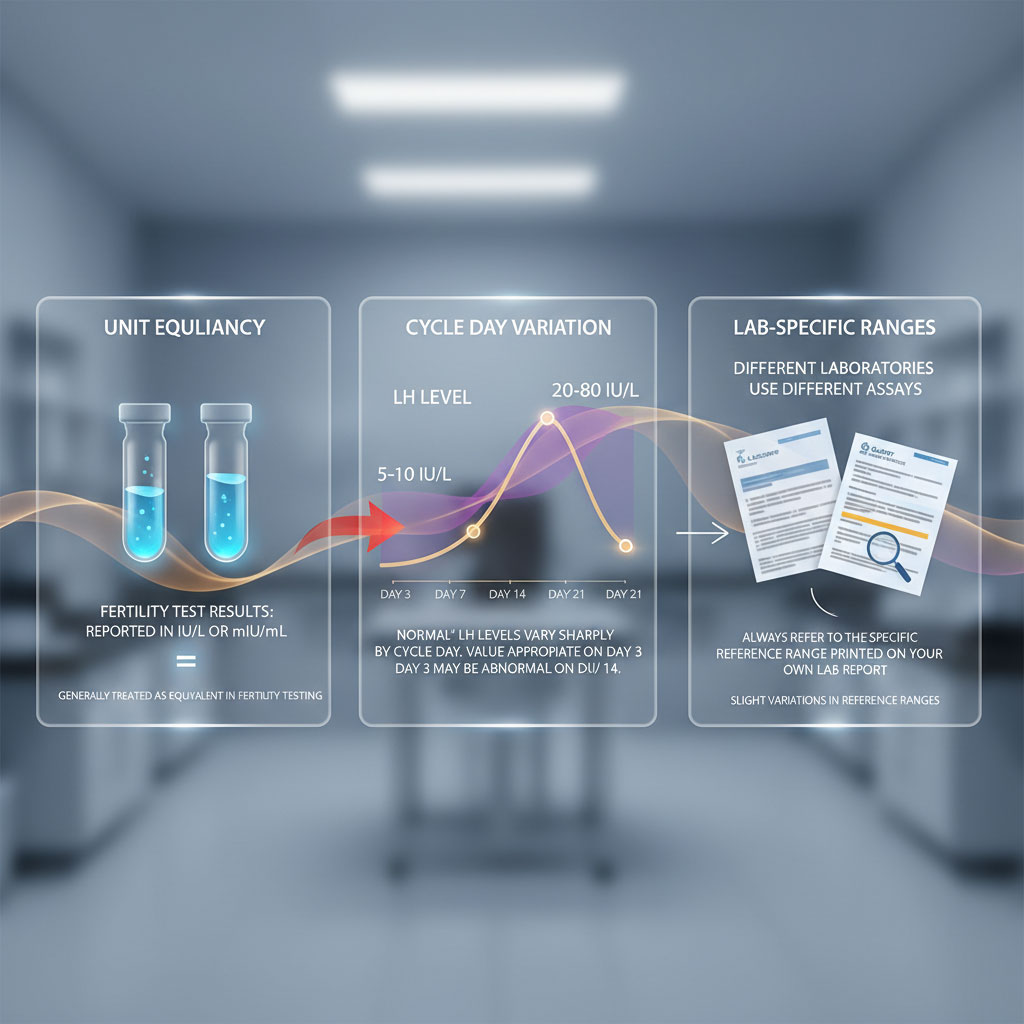
Understanding what constitutes a “normal” range is difficult because these numbers change drastically depending on where you are in your cycle. A level that is “normal” on day 3 would be diagnostically concerning on day 14. Furthermore, different laboratories (like LabCorp vs. Quest) use different assays, so reference ranges can vary slightly. Always refer to the reference range printed on your specific lab report.
The Follicular Phase (Pre-Ovulation)
During the early part of your cycle, known as the follicular phase (roughly days 1–13 in a 28-day cycle), normal LH levels should be relatively low.
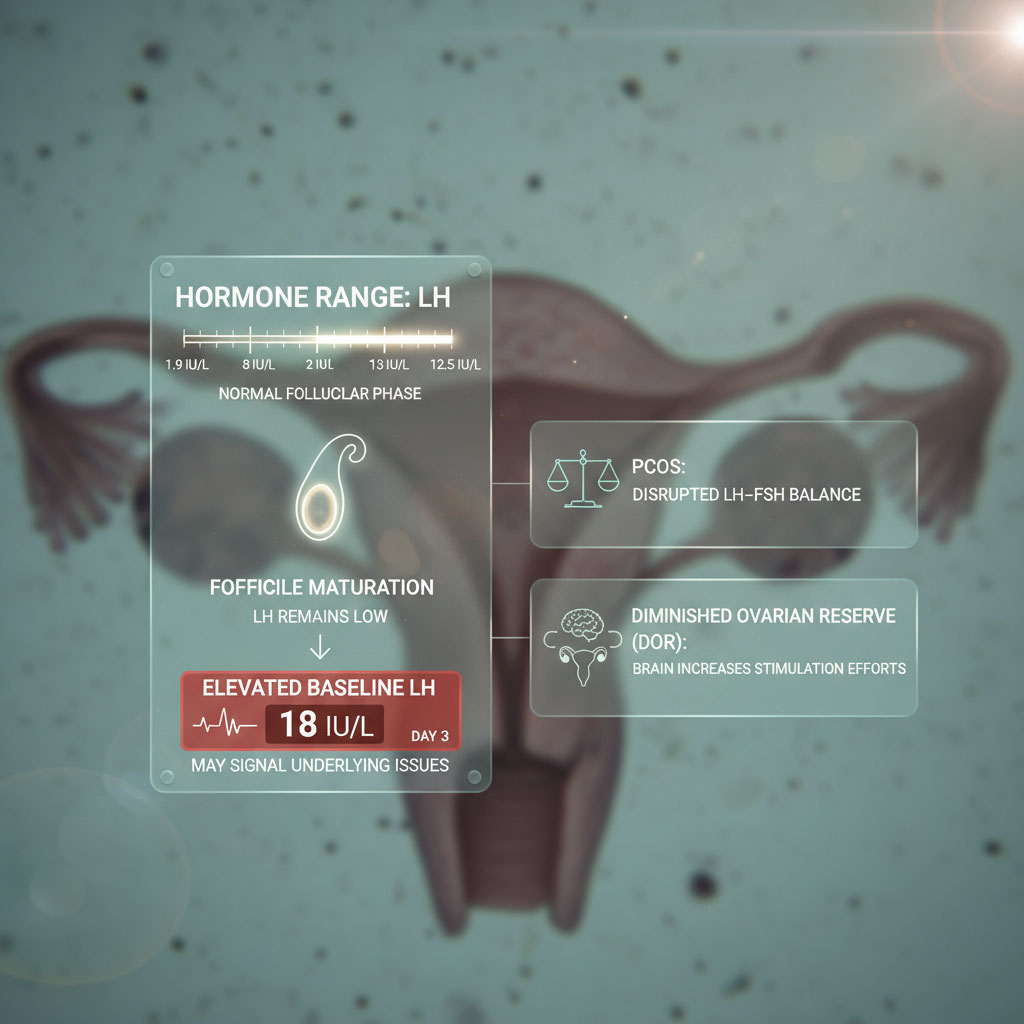
- Standard Clinical Range: 1.9 to 12.5 IU/L
During this time, your body is focusing on maturing the follicle, not releasing it. If your baseline LH is significantly higher than this range before your expected window (for example, resting at 15 or 20 IU/L on day 3), it could indicate an underlying issue. Consistently elevated baseline levels are a hallmark of conditions like PCOS (Polycystic Ovary Syndrome), where the delicate balance between LH and FSH is disturbed, or may indicate diminished ovarian reserve (DOR), where the brain has to work harder to stimulate the ovaries.
The Mid-Cycle Peak (The Surge)
This is the moment you are looking for. During the surge, LH hormone levels skyrocket.
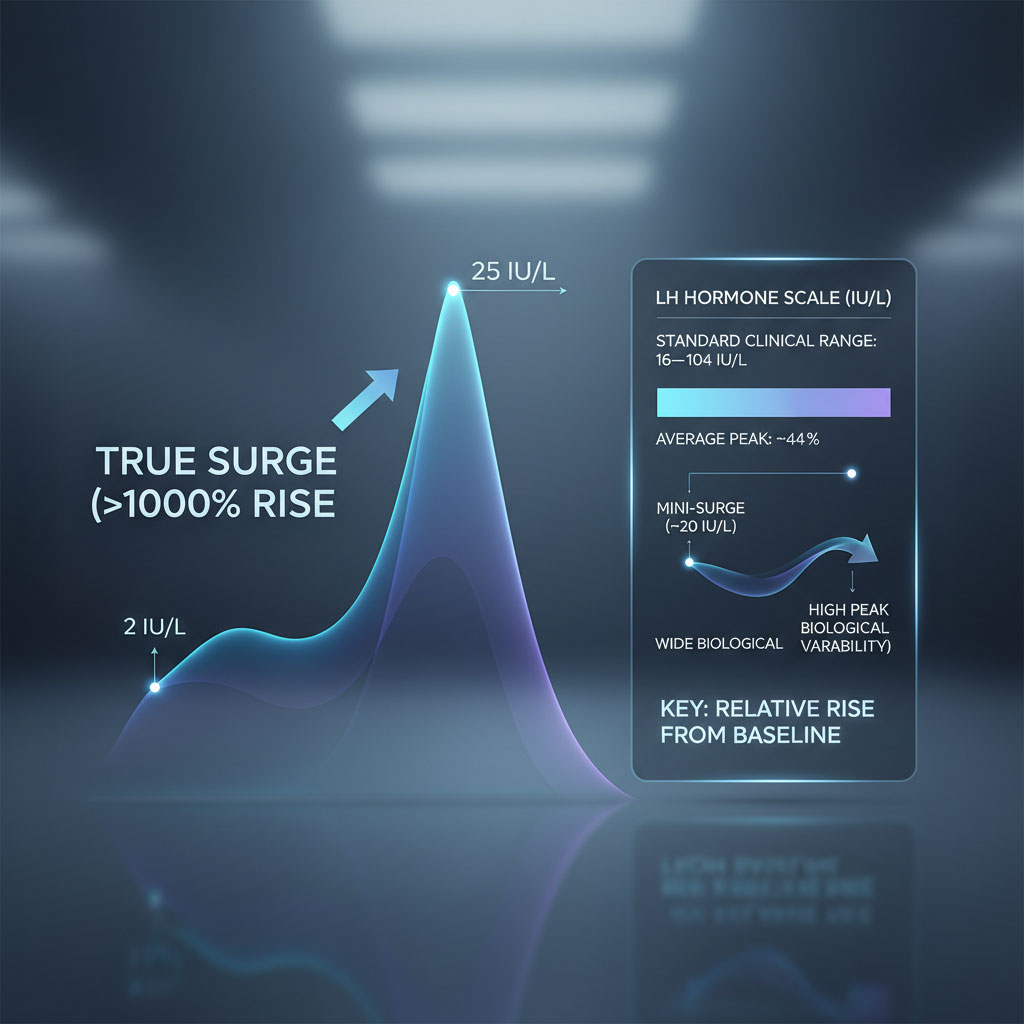
- Standard Clinical Range: 16 to 104 IU/L
- Average Peak: ~44 IU/L
The “normal” range here is incredibly wide. This is because biological diversity is significant. Some women ovulate successfully with a “mini-surge” peak of 20 IU/L, while others see numbers climb over 80 IU/L or even 100 IU/L. The most important factor is not just the absolute height of the number, but the relative rise compared to your personal baseline. A jump from 2 IU/L to 25 IU/L is a significant surge (over a 1000% increase), even if it doesn’t reach the higher end of the clinical range.
The Luteal Phase (Post-Ovulation)
Once ovulation has occurred, LH levels drop rapidly.
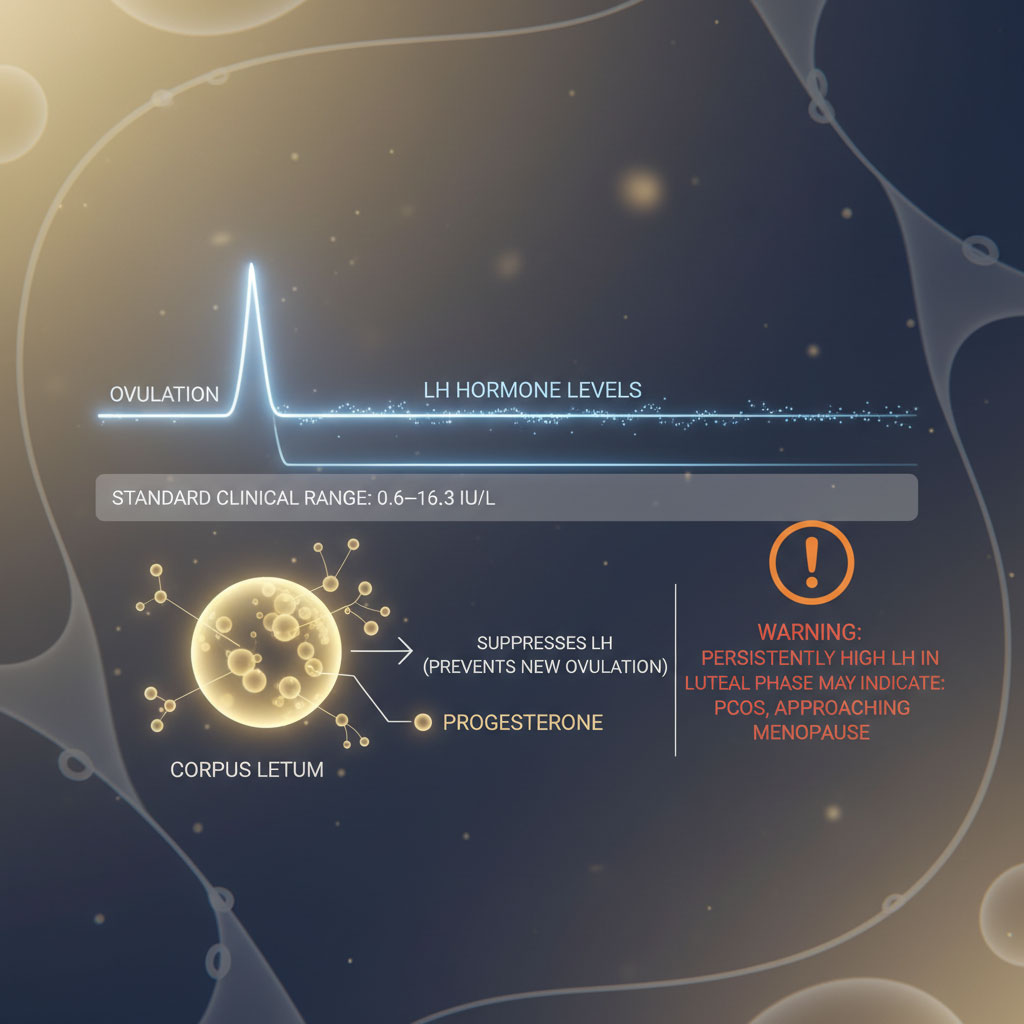
- Standard Clinical Range: 0.6 to 16.3 IU/L
This drop is necessary because the corpus luteum (the shell of the released egg) begins producing progesterone to support a potential pregnancy. Progesterone suppresses LH production to prevent another ovulation event during the same cycle. If LH stays high during this phase, it may suggest hormonal dysregulation, such as PCOS or approaching menopause.
Menopause and LH Levels
For women entering perimenopause or menopause, LH levels behave differently. Because the ovaries stop producing estrogen and releasing eggs, the negative feedback loop breaks. The brain, sensing low estrogen, keeps shouting at the ovaries to work, pumping out more and more LH in a futile attempt to stimulate activity.
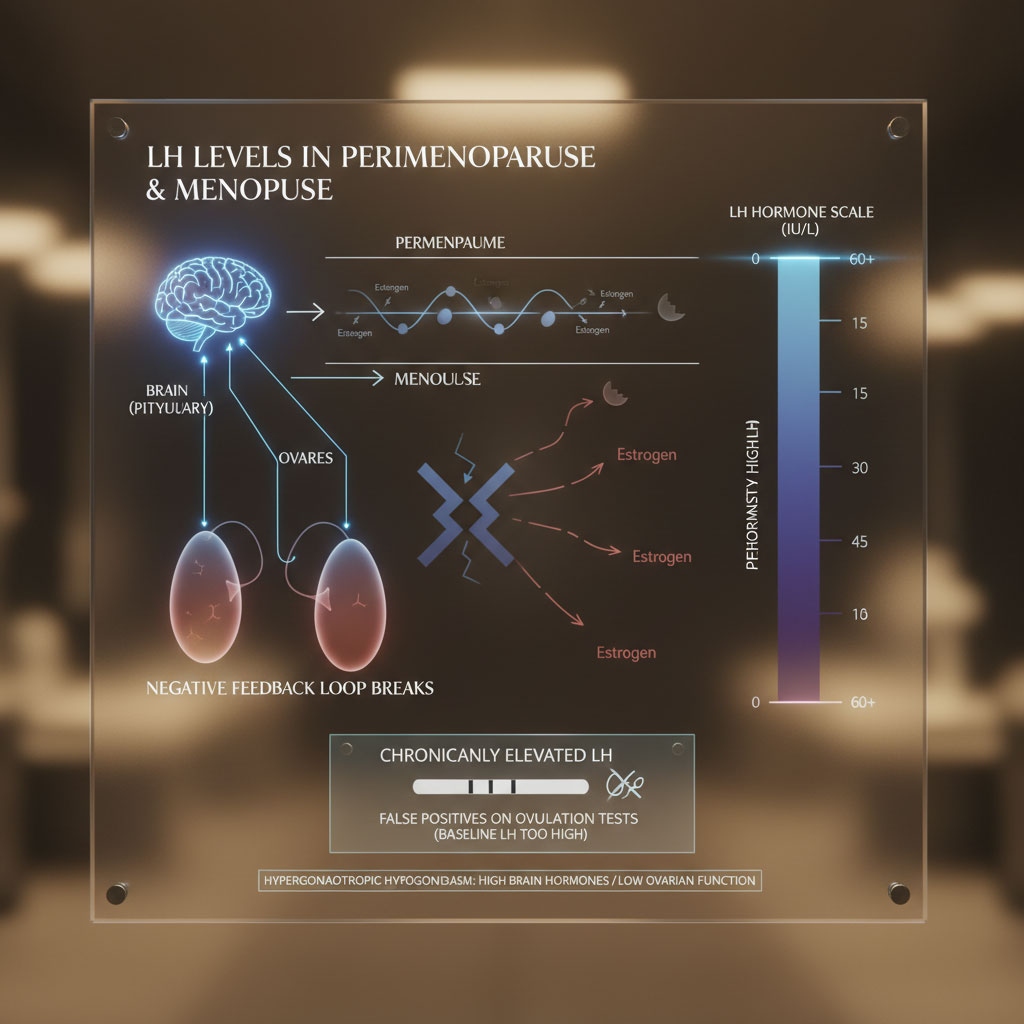
- Standard Clinical Range: 15 to 60+ IU/L
This is why perimenopausal women often get false positives on ovulation tests; their baseline LH is high enough to trigger the dye, even if they are not ovulating. It represents a state of “hypergonadotropic hypogonadism”—high brain hormones, low ovary function.
Reference Table: Normal LH Ranges by Cycle Phase
Below is a detailed breakdown of standard LH hormone levels based on US clinical laboratory guidelines. These ranges serve as a general benchmark for interpreting your fertility data.
| Menstrual Cycle Phase | Normal LH Range (IU/L) | Physiological Event | Key Takeaway |
| Early Follicular | 1.9 – 12.5 IU/L | Egg Recruitment | Baseline level; should remain low to allow follicle growth. |
| Mid-Cycle (Surge) | 16.0 – 104.0 IU/L | Ovulation Trigger | The “Peak” fertility moment; levels spike rapidly. |
| Luteal Phase | 0.6 – 16.3 IU/L | Post-Ovulation | Levels drop as Progesterone rises to prepare the lining. |
| Pregnancy | < 1.5 IU/L | Gestation | LH is suppressed by hCG to prevent further ovulation. |
| Menopause | 15.0 – 62.0+ IU/L | Ovarian Cessation | Persistently high due to lack of estrogen feedback. |
Practical Strategies: Detecting Your Surge with Accuracy
Knowing the clinical numbers is one thing, but catching the surge at home requires the right tools, timing, and technique. The market is flooded with ovulation tests and OPKs (Ovulation Predictor Kits), but using them correctly is often more difficult than manufacturers imply. A missed surge is often due to user error or timing issues rather than a biological failure.
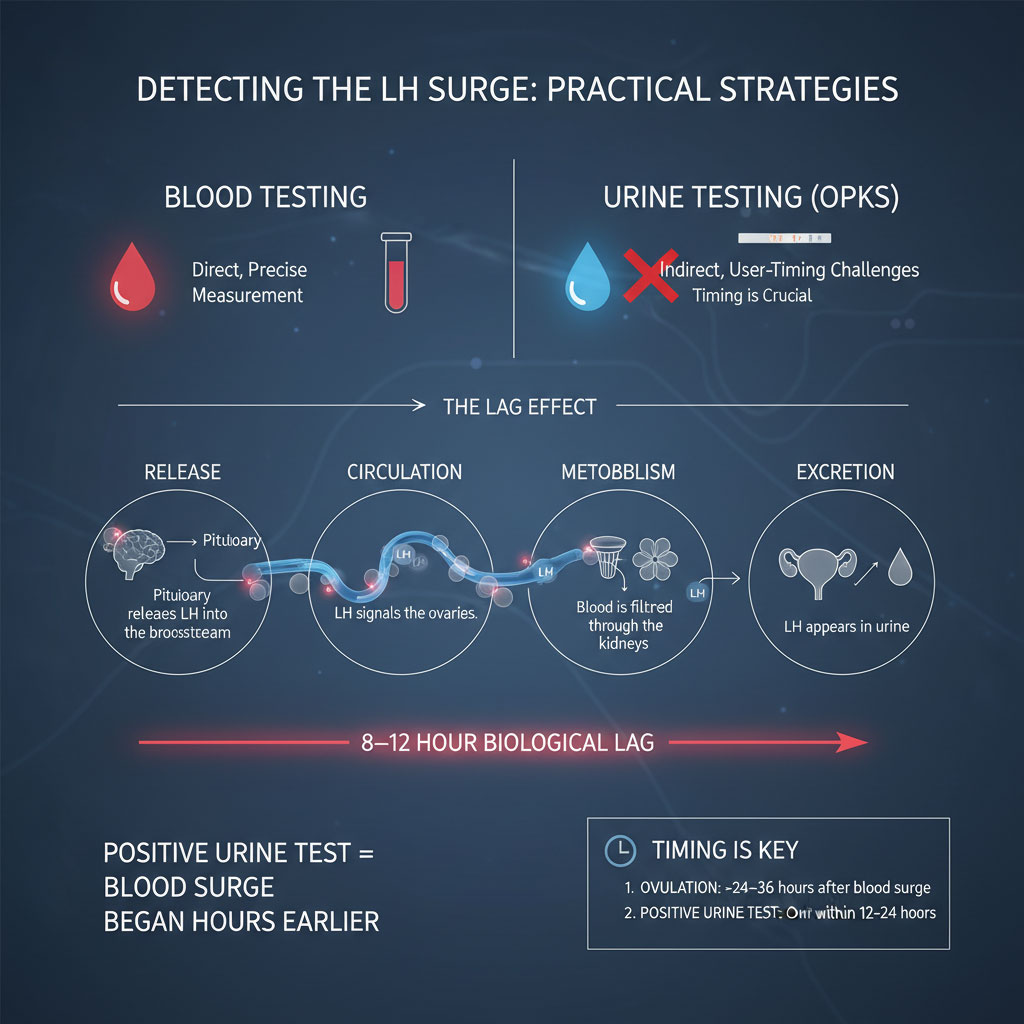
The “Lag Effect”: Blood vs. Urine Testing
The gold standard for measuring LH levels is a blood test drawn at a clinic. This detects the surge the moment the hormone enters your bloodstream from the pituitary gland. However, daily blood draws are impractical and expensive for most women. This is why most rely on urine-based ovulation tests.
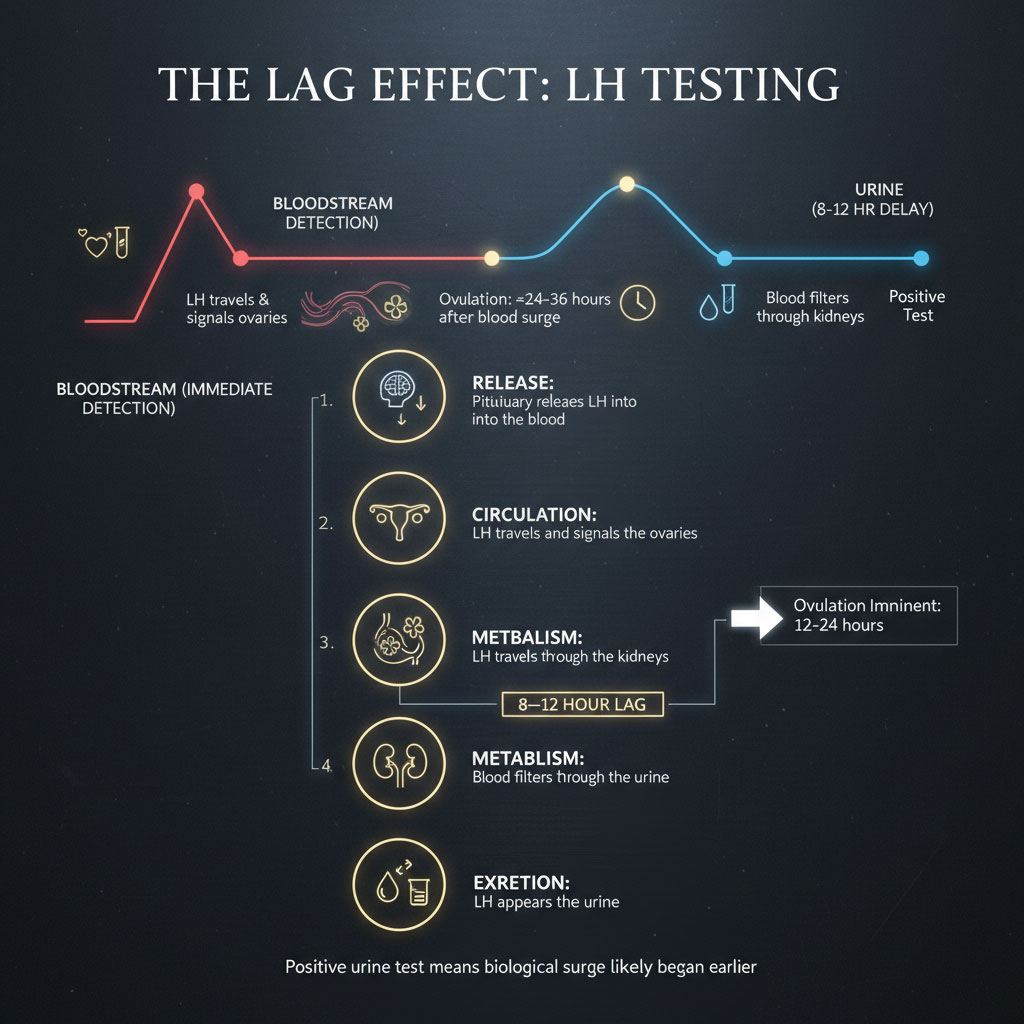
It is critical to understand the biological lag between blood and urine.
- Release: The pituitary releases LH into the blood.
- Circulation: The hormone circulates, signaling the ovaries.
- Metabolism: The blood filters through the kidneys.
- Excretion: The LH is processed and excreted in urine.
This process can take 8 to 12 hours. This means that by the time you get a positive result on a urine ovulation test, your biological surge might have started half a day ago. This lag actually helps with timing intercourse. Since ovulation happens roughly 24 to 36 hours after the blood surge, a positive urine test means ovulation is imminent, usually occurring within the next 12 to 24 hours.
Best Time to Test: Why Morning Isn’t Best
Because of this metabolic lag, testing with “first morning urine” (FMU) is not recommended for LH tracking, unlike pregnancy testing which relies on concentrated hCG.
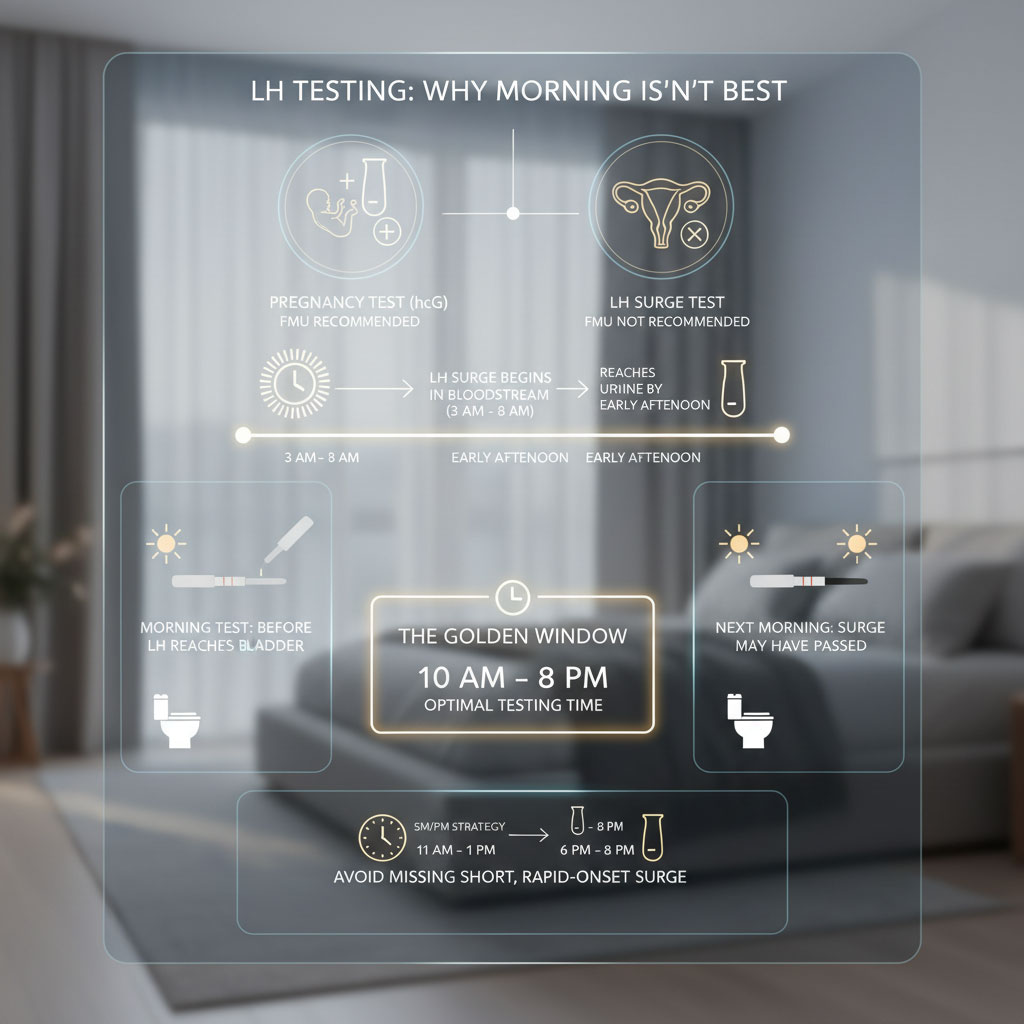
Most LH surges begin in the bloodstream in the early morning hours (between 3 AM and 8 AM). By the time the hormone is processed and reaches your urine, it is often early afternoon. If you test at 6 AM, you might test before the surge has reached your bladder. By the next morning at 6 AM, the surge might be over.
The Golden Window: The best time to test is typically between 10 AM and 8 PM.
- The SM/PM Strategy: Many women trying to catch a rapid surge will test twice a day. Once around 11:00 AM – 1:00 PM and once around 6:00 PM – 8:00 PM. This strategy ensures you do not miss a short surge (known as a “rapid onset” surge) that might appear and disappear between daily testing sessions.
The “Hold” Technique
Hydration plays a major role in the accuracy of urine tests. If you drink excessive amounts of water before testing, you may dilute your urine to the point where the LH concentration is undetectable, even if you are surging.
- Recommendation: Perform a 2 to 3-hour “hold.” Limit fluid intake and avoid urinating for roughly two hours before taking the test. This allows the hormone to build up in the bladder, providing a more accurate reflection of your blood levels. You do not need to dehydrate yourself, but avoid chugging a liter of water right before you test.
Troubleshooting: The “Hook Effect”
In very rare cases, if your LH levels are incredibly high (well over 100 IU/L), you might experience the “Hook Effect.” This is a phenomenon where there are so many hormone molecules that they overwhelm the antibodies on the test strip, preventing them from binding correctly and forming the “sandwich” needed to show the colored line. This results in a falsely light or negative line. If you suspect you are surging (based on cervical mucus or ovulation pain) but getting negatives, diluting your urine with 50% water and re-testing can sometimes reveal the true positive line.
A Guide to Ovulation Test Technologies
You have three main choices for tracking your fertile window at home, each offering a different level of detail and suitability for different lifestyles.
1. Standard Analog Strips (The Budget Option)
These are the simple paper strips often bought in bulk (brands like Wondfo or Easy@Home).
- How they work: They use a threshold (usually 25 mIU/mL).
- Interpretation: The test is only positive if the test line is as dark as or darker than the control line.
- Pros: Inexpensive (cents per strip), allowing for frequent testing (3-4 times a day) without breaking the bank.
- Cons: Visual interpretation can be subjective. “Is this line dark enough?” is a common source of stress for users. This is often called “line progression analysis.”
2. Digital Ovulation Tests (The User-Friendly Option)
Brands like Clearblue use a digital reader to interpret the lines for you.
- How they work: They establish a baseline by testing early in the cycle. They often show a “flashing smiley” when estrogen rises (high fertility) and a “solid smiley” when the LH surge is detected (peak fertility).
- Pros: No squinting at lines; clear “Yes/No” result. It tracks two hormones (estrogen and LH), giving you a larger fertile window (usually 4 days).
- Cons: Expensive. Also, if you have PCOS and your LH is always slightly elevated, you may get endless “high fertility” days without ever getting a “peak,” as the algorithm gets confused by the high baseline.
3. Quantitative Analyzers (The Data-Driven Option)
Newer tech devices like Mira or Inito represent the future of home fertility tracking.
- How they work: These systems use a digital wand and a smartphone app to give you an exact number in IU/L using fluorescence technology.
- Pros: Instead of a binary “positive/negative,” you see the full curve. You can see if your LH surge hit 25 IU/L or 65 IU/L. This is vital for women with irregular cycles or PCOS who need to see the nuance of their hormone levels to distinguish a small fluctuation from a true surge.
- Cons: High entry cost for the device and expensive test wands.
Interpreting “Abnormal” Levels: What Do They Mean?
Sometimes, you might track for weeks and never see a surge. Other times, your LH levels might stay high all month. These patterns can provide vital clues about your underlying reproductive health and are worth discussing with a reproductive endocrinologist.
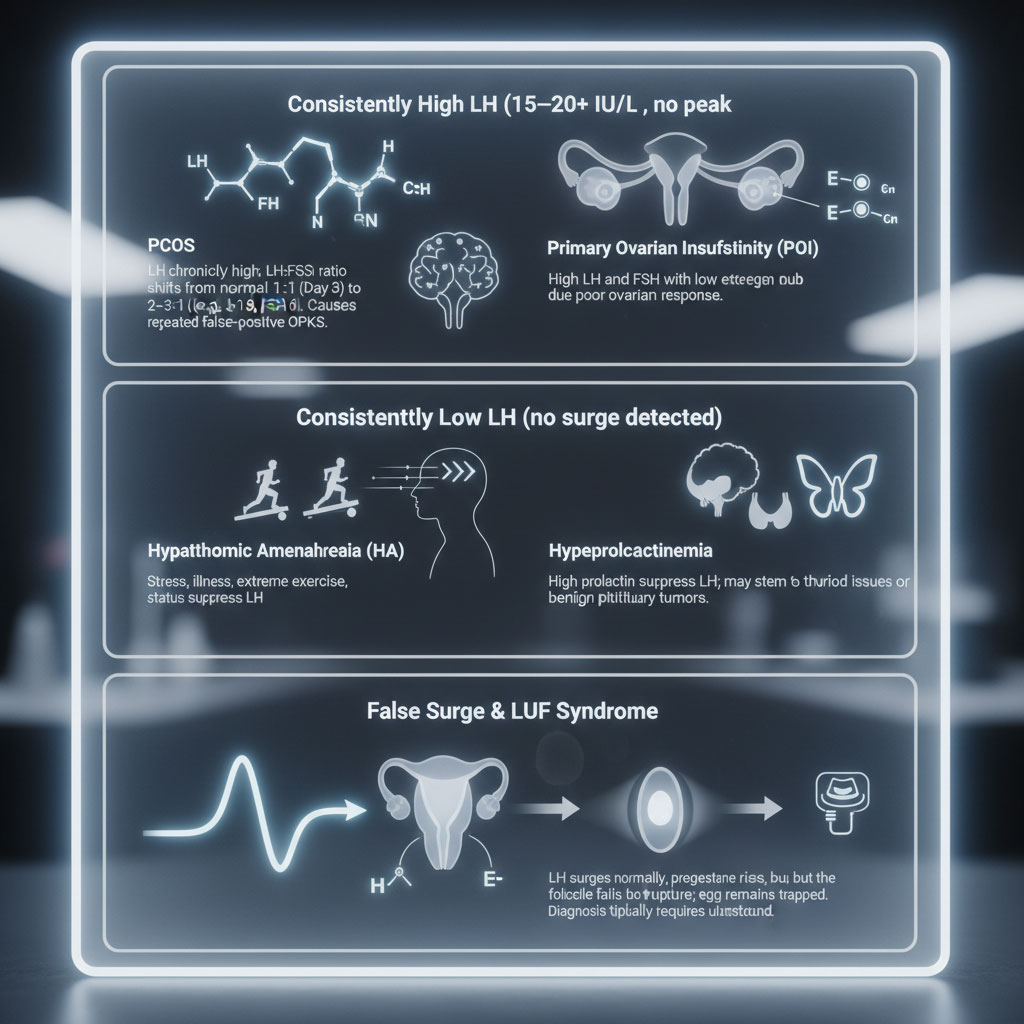
Consistently High LH Levels (No Surge Pattern)
If your LH hormone levels remain elevated (consistently above 15 or 20 IU/L) throughout your cycle without a distinct peak and drop, your body might be struggling to ovulate.
The PCOS Connection:
Women with Polycystic Ovary Syndrome (PCOS) often have a hormonal imbalance where LH is chronically high. Doctors look at the LH to FSH ratio.
- Normal: In the early follicular phase (Day 3), FSH and LH are roughly 1:1.
- PCOS: LH is often two or three times higher than FSH (e.g., LH is 18, FSH is 6).
This constant elevation can confuse standard OPKs, causing them to show positive or near-positive results multiple times a month even if no egg is released. This is why women with PCOS often find standard strips frustrating and inaccurate; they never get a true “negative” to compare against.
Primary Ovarian Insufficiency (POI):
If LH is high but you are not near typical menopause age, it could indicate POI (formerly known as Premature Ovarian Failure). In this condition, the brain is shouting at the ovaries to produce eggs, but the ovaries are not responding due to low egg reserve or dysfunction. This results in high LH and FSH levels combined with low estrogen.
Consistently Low LH Levels (No Surge Detected)
If you never see a positive ovulation test and your lines are always very faint or invisible, you may be experiencing an anovulatory cycle. This means you are bleeding (having a period), but you are not releasing an egg.
Hypothalamic Amenorrhea (HA):
This is a functional issue often caused by lifestyle factors. Common causes include chronic stress, significant illness, extreme exercise (like marathon training), or being underweight/undereating. In this state, the hypothalamus perceives the environment as “unsafe” for pregnancy and turns down the dial on luteinizing hormone production to conserve energy. The surge simply never triggers.
Hyperprolactinemia:
High levels of prolactin (the breastfeeding hormone) can suppress LH. This can be caused by thyroid issues or benign pituitary tumors.
The “False Surge” and LUF Syndrome
Rarely, you might catch a perfect LH surge on a test but still not get pregnant. One possibility is Luteinized Unruptured Follicle (LUF) syndrome.
In this case, the hormones surge correctly, and the cells surrounding the egg luteinize (start making progesterone). However, the follicle wall is too thick or tough to rupture, or the signaling mechanism fails. The egg remains trapped.
Because progesterone is produced, you will still see a temperature shift on a BBT chart, and you will get a period at the normal time. This condition is notoriously difficult to diagnose and usually requires ultrasound monitoring during the ovulation window to see if the follicle actually collapsed or if it remained intact.
Latest Industry Trends: Surge Profiles & AI
The world of fertility tracking is evolving rapidly. We are moving away from simple calendar methods (the “Rhythm Method”) and toward data-driven precision that accounts for individual biological variations.
Surge Profiles: The “Shape” of Your Surge
Recent data from millions of cycles tracked on apps like Premom and Mira have revealed that not all LH surges look the same. Understanding your specific pattern can help you time intercourse better and reduce anxiety.
- The Rapid Onset Surge:
Some women have an LH spike that lasts less than 10 hours. It rises fast and falls fast. If you test only once a day in the morning, you might miss it entirely. This profile is the primary reason why twice-daily testing is recommended for women who struggle to “catch” their peak. - The Gradual Surge:
Other women see LH levels rise slowly over 3 to 4 days before hitting peak fertility. This gives you plenty of warning that ovulation is approaching, allowing you to time intercourse comfortably over several days. - The Double Peak:
A smaller percentage of women experience a “false start.” LH rises, dips for a day, and then surges again. Usually, ovulation occurs after the second, stronger peak. This highlights the importance of continuing to test even after you think you have seen a peak, especially if your basal body temperature shift hasn’t happened yet. - The Plateau:
Some women, particularly those with higher baseline hormones, see an elevated level that sustains for 2 or 3 days before dropping. This is still considered a valid surge, and ovulation typically occurs after the initial rise of the plateau.
AI in Fertility Tracking
Artificial Intelligence is now being integrated into fertility apps to provide personalized insights. By analyzing your past cycle data, normal LH levels, and the color intensity of photos you take of your test strips, these apps can predict your fertile window with greater accuracy than simple calendar math.
They can recognize your personal baseline. If your baseline is usually 5 IU/L and it jumps to 15 IU/L, the AI might flag this as the start of your surge, even if a standard test wouldn’t call it positive yet (because it hasn’t hit 25 IU/L). This technology allows for a customized approach to conception that was previously only available in a clinical setting.
Lifestyle Factors: Optimizing Your LH Levels
While genetics play a huge role in your hormone levels, lifestyle factors can influence the regularity and strength of your LH surge.
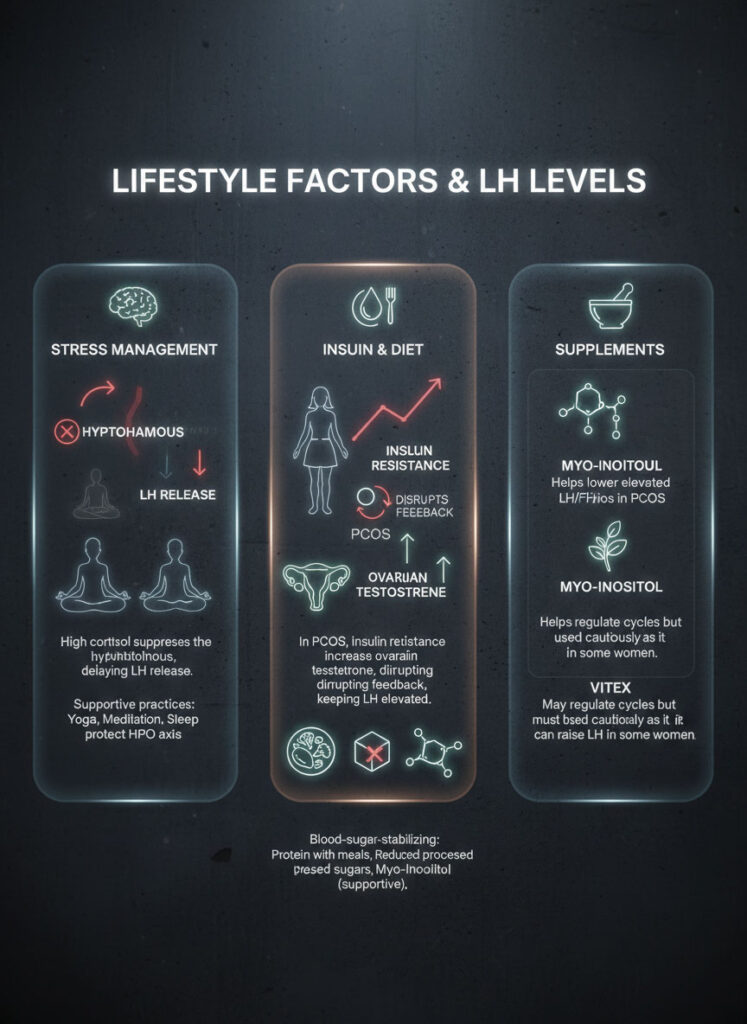
Stress Management
Cortisol, the stress hormone, acts as a bully to the reproductive system. High cortisol levels can suppress the hypothalamus, delaying the signal to release LH. This is why “stress delaying ovulation” is a biological reality, not just an old wives’ tale. Practices like yoga, meditation, or simply ensuring adequate sleep can help lower cortisol and protect the HPO axis.
Insulin and Diet
For women with PCOS, insulin resistance is a key driver of high LH levels. High insulin prompts the ovaries to produce testosterone, which disrupts the feedback loop and keeps LH elevated. Dietary changes that stabilize blood sugar—such as eating protein with every meal, reducing processed sugars, and considering supplements like Myo-Inositol—have been shown to help normalize LH levels and restore spontaneous ovulation in many women.
Supplements
- Myo-Inositol: Widely researched for helping to lower high LH/FSH ratios in PCOS patients.
- Vitex (Chasteberry): Often used to regulate cycles, though it should be used with caution and under provider guidance, as it can sometimes raise LH levels, which might be counterproductive if yours are already high.
Comparison of Ovulation Test Technologies
Choosing the right tool depends on your budget, your lifestyle, and your cycle regularity. The table below compares the most popular options available in the USA to help you decide which method suits your needs.
| Feature | Standard OPK Strips (e.g., Wondfo) | Digital Tests (e.g., Clearblue) | Quantitative Analyzers (e.g., Mira/Inito) |
| Output Format | Two Lines (Visual Interpretation) | Smiley Face (Icon Based) | Exact Hormone Value (e.g., 25 IU/L) |
| Accuracy | ~99% (Dependent on user eye) | >99% (Digital interpretation) | Lab-grade equivalent precision |
| Cost | Low (Approx $0.30 per test) | Medium (Approx $2.00 per test) | High ($40+ for device, high strip cost) |
| Best For | Women with regular cycles on a budget | Ease of use; confirming peak fertility | Women with PCOS, irregular cycles, or data lovers |
| Detection Range | Threshold based (usually 25 mIU/mL) | Threshold based (often 40 mIU/mL) | Full range detection (1 to 100+ IU/L) |
Summary & Key Takeaways
Navigating the world of fertility hormones can feel overwhelming, but the data tells a clear story. A normal LH surge is the definitive sign that your body is preparing to release an egg. For most women, this surge reaches a level between 16 and 104 IU/L and triggers ovulation within 24 to 36 hours.
If you are using ovulation tests, remember that a positive result is a green light for your fertile window. Look for that test line to be as dark as the control. If your LH levels seem consistently off—either too high due to conditions like PCOS or too low due to hypothalamic suppression—it serves as a valuable signal to consult a doctor.
By understanding your personal patterns and using the right tools, you move from guessing to knowing. You can stop wondering if your timing is right and start relying on the biological data your body provides every month. Whether you use simple strips or advanced AI analytics, the goal remains the same: identifying that crucial window of opportunity to help you build your family.
Frequently Asked Questions (FAQs)
How soon after the LH surge do you ovulate?
You will typically ovulate 24 to 36 hours after the onset of the LH surge (when levels first start to rise significantly). If you identify the peak (the highest point of the surge), ovulation usually follows within 10 to 12 hours. This makes the day of the surge your day of peak fertility and the most important time for intercourse.
What is a normal LH level for a woman trying to conceive?
During the follicular phase, normal baseline levels are between 1.9 and 12.5 IU/L. During the mid-cycle surge, levels should spike significantly, usually falling between 16 and 104 IU/L. However, a surge generally needs to reach at least 20-25 IU/L above your personal baseline to trigger ovulation effectively.
Can you have an LH surge and not ovulate?
Yes. This is known as Luteinized Unruptured Follicle (LUF) syndrome. In this scenario, your body produces the LH surge correctly, but the egg is not released from the ovary. You may still get a regular period and even see a temperature shift, making this condition difficult to diagnose without ultrasound monitoring.
Why is my LH level always high?
Persistently high LH hormone levels often indicate PCOS (Polycystic Ovary Syndrome) or perimenopause. In PCOS, the ratio of LH to FSH is often elevated (greater than 2:1), which can cause false positive results on ovulation tests throughout the month. In perimenopause, the brain produces excess LH to try to stimulate aging ovaries.
Is a faint line on an ovulation test a positive result?
No. Unlike a pregnancy test where any line counts, a faint line on an OPK is considered negative. This simply detects your baseline luteinizing hormone, which is always present in low amounts. For a test to be positive, the test line must be as dark as or darker than the control line.
What time of day is best to take an ovulation test?
The best time to test is typically between 10 AM and 8 PM. The LH surge often begins in the blood in the morning but takes several hours to appear in your urine. Testing in the early afternoon helps catch the surge that started earlier that day. Avoid first morning urine unless the specific test instructions state otherwise.
Do digital ovulation tests work for women with PCOS?
Digital tests can be challenging for women with PCOS. Because these tests rely on a set threshold or a baseline algorithm, the chronically high LH levels associated with PCOS can confuse the device. This often leads to many days of “flashing smileys” (high fertility) without ever getting a “solid smiley” (peak), or false peaks. Quantitative tests are often better for PCOS.
Does LH drop immediately after ovulation?
Yes. Once ovulation occurs, LH levels drop rapidly as the luteal phase begins. Progesterone then becomes the dominant hormone to support the uterine lining. If LH remains high after ovulation, it warrants medical investigation to rule out hormonal imbalances.
Can stress delay my LH surge?
Yes. Stress triggers the release of cortisol, which can suppress the hypothalamus. This disruption can delay or even prevent the signal to the pituitary gland, causing your LH surge to happen later than expected or not at all for that cycle. This is why cycles can vary in length during stressful periods or travel.
What is the difference between LH and hCG tests?
LH tests predict ovulation, while hCG tests confirm pregnancy. However, the two hormones are molecularly very similar (they share an alpha subunit). High levels of LH can sometimes turn a pregnancy test positive (rarely), and high levels of hCG (pregnancy) can turn an ovulation test positive. Always use the correct test for your specific goal.
Does the intensity of the line matter if it is not peak?
In quantitative tracking, yes. A rise from a baseline of 5 IU/L to 15 IU/L indicates estrogen is likely rising and your window is opening. On standard strips, however, any line lighter than the control is generally treated as “negative” until it crosses the threshold, though savvy users often watch for the gradient to darken (the “progression”) to anticipate the peak.
How do I calculate my fertile window using LH?
Your fertile window includes the 5 days before ovulation and the day of ovulation itself. Since the LH surge happens 24-36 hours before the egg is released, a positive test signals you are in the final, most fertile 1-2 days of that window. Combining LH testing with observing cervical mucus (which appears days before the surge) can give you an even broader picture of your fertility.








