When that sharp, unrelenting pain strikes the lower left side of your abdomen, your immediate priority is relief. You know something is wrong. The bloating feels different, the tenderness is localized, and the thought of eating a heavy meal is physically repulsive. This is the reality of an acute flare-up. For thousands of Americans every year, this moment marks the beginning of a strict but necessary recovery phase known as bowel rest.
Table of Contents
A liquid diet for diverticulitis is a temporary medical intervention designed to provide “bowel rest” during an acute flare-up. By consuming only clear fluids like bone broth, pulp-free juices, and electrolyte-rich drinks for 48 to 72 hours, you significantly reduce colonic pressure. This staged approach allows the inflamed sigmoid colon to heal before you gradually transition back to low-fiber solids as abdominal pain subsides.
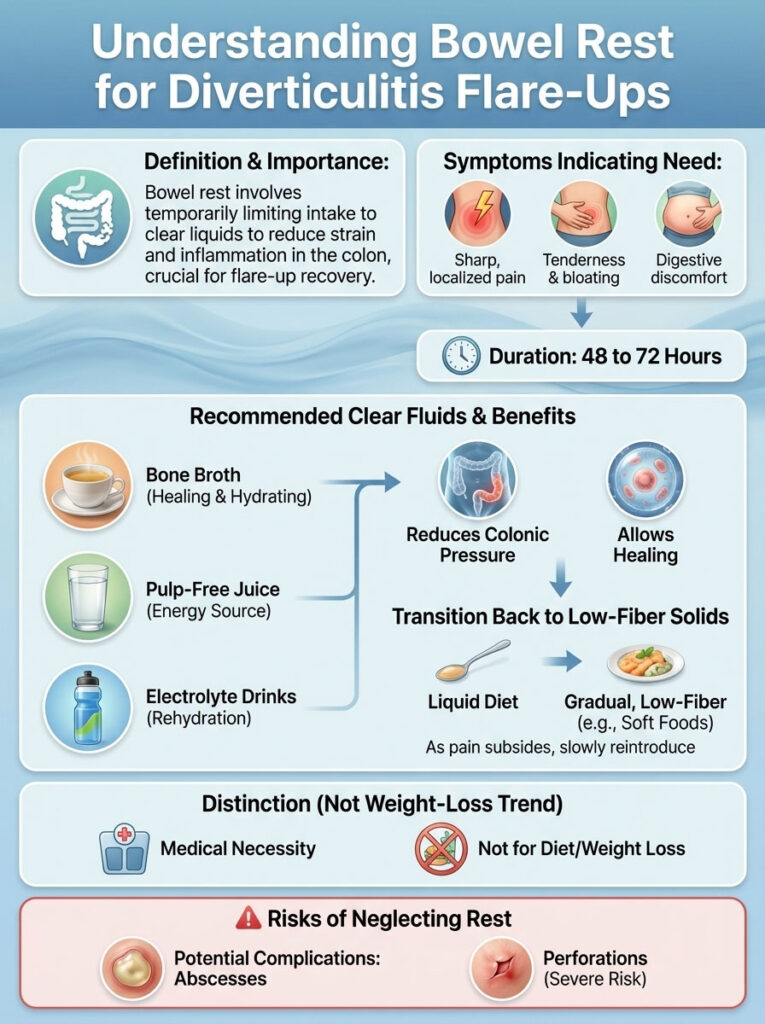
This is not a weight-loss trend or a detox fad. It is a strategic medical protocol used to prevent complications like abscesses or perforations. If you are navigating a flare-up at home, knowing exactly what to drink for diverticulitis pain can be the difference between a manageable recovery and a trip to the emergency room.
The Medical Science of Bowel Rest for Inflamed Diverticula
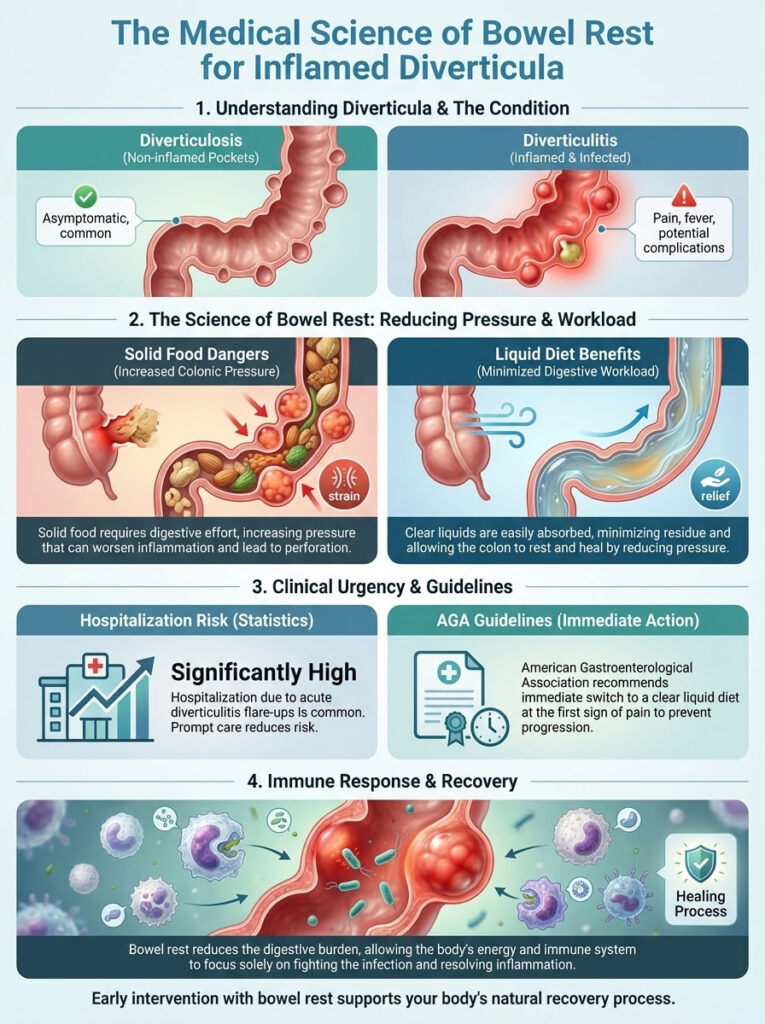
To understand why you must stop eating solid food, you have to understand the mechanics of the condition. Diverticula are small, bulging pouches that can form in the lining of your digestive system. They are most common in the lower part of the large intestine, known as the sigmoid colon. When these pouches exist without issue, it is called diverticulosis. When they become inflamed or infected, it becomes diverticulitis.
Reducing Colonic Pressure and Workload
The primary goal of a liquid diet for diverticulitis is to reduce the volume of fecal matter passing through the large intestine. Solid foods, especially those high in fiber, create bulk. During a healthy state, bulk is good. During an infection, bulk forces the colon to contract vigorously to move waste. These contractions increase pressure on the already inflamed pouches.
By switching to a clear liquid diet, you reduce this workload to near zero. The American Gastroenterological Association (AGA) guidelines suggest that for uncomplicated diverticulitis, this reduction in pressure allows the inflammation to subside naturally.
Preventing Complications and Hospitalization
Statistics from the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) indicate that approximately 200,000 people in the United States are hospitalized for diverticulitis annually. Many of these cases escalate because the patient continues to eat solids during the early stages of pain. Immediate adherence to a diverticulitis flare up diet focused on liquids can often arrest the progression of the infection, allowing the body’s immune system to fight the inflammation without the added stress of digestion.
Stage 1: The Clear Liquid Diet Protocol (First 48–72 Hours)
The “Red Zone” of recovery is the first 2 to 3 days. This is when pain is most acute, and fever may be present. During this window, your intake must be strictly limited to liquids you can see through. If the liquid contains pulp, cream, or solid particles, it is forbidden.

High-Quality Bone Broth for Diverticulitis Recovery
Not all broths are created equal. While a simple bouillon cube can provide sodium, a high-quality bone broth for diverticulitis offers superior benefits. Brands like Pacific Foods or Kettle & Fire produce broths rich in natural collagen and amino acids like glutamine.
Glutamine is a critical fuel source for the cells lining the intestinal wall. Sipping warm bone broth provides essential nutrition that supports gut lining repair without requiring mechanical digestion. It is gentle, soothing, and vastly superior to water alone.
Essential Beverages and Pulp-Free Juices
Hydration is your primary defense against the constipation that often follows a flare-up. You should aim for 8 to 12 cups of fluid daily. However, the type of juice matters.
- Apple Juice: A staple of the clear liquid diet. It provides glucose for energy and is generally well-tolerated.
- White Grape Juice: Another safe option that is less acidic than other fruit juices.
- Cranberry Juice: Ensure it is a juice cocktail or blend that does not contain high amounts of pulp or sediment.
You must avoid orange juice with pulp, prune juice, or pineapple juice during this stage. The fiber content in these can stimulate bowel contractions, which is exactly what you are trying to avoid.
The “Newspaper Rule” for Liquid Selection
A practical way to determine if a drink is safe for Stage 1 is the “Newspaper Rule.” Pour the liquid into a clear glass. Hold a newspaper or a piece of text with large print behind the glass. If you can read the letters through the liquid, it is safe to consume. If the liquid is cloudy, opaque, or blocks the text, it belongs in Stage 2 or 3, not Stage 1.
Electrolyte Replacement and Hydration
Fever and diarrhea often accompany a flare-up, leading to rapid dehydration. Water is essential, but it does not replace lost minerals.
- Pedialyte: This is a medical-grade option often recommended because it has a higher electrolyte content and less sugar than sports drinks.
- Gatorade or Powerade: These are acceptable for electrolyte replacement, but be mindful of the sugar content. The “Zero” versions are often better if you are sensitive to high sugar intake, though some artificial sweeteners can cause minor gas.
Comparison: Clear Liquid vs. Full Liquid Diet
One of the most common sources of confusion is distinguishing between a clear liquid diet and a full liquid diet. Moving to full liquids too soon can re-trigger pain. Moving too late can lead to unnecessary weakness and muscle loss.

| Feature | Clear Liquid Diet (Stage 1) | Full Liquid Diet (Stage 2) |
| Timing | First 24–72 hours of acute pain. | Days 3–5 (once pain decreases signficantly). |
| Visual Test | Transparent. Must see through it. | Opaque. Can be creamy or thick. |
| Protein Source | Negligible (Amino acids in broth). | High (Dairy, strained meats, protein powders). |
| Permitted Foods | Broth, tea, apple juice, plain Jell-O. | Milk, yogurt (no fruit), Ensure, strained cream soups. |
| Key Goal | Total bowel rest and hydration. | Caloric maintenance and nutritional support. |
| Fiber Content | Zero residue. | Minimal residue. |
| Diverticulitis Impact | Maximize rest for sigmoid colon. | Begin engaging digestion gently. |
Stage 2: Transitioning to a Full Liquid Diet (Nutrition Recovery)
Once your fever has broken and your abdominal tenderness has shifted from a sharp stab to a dull ache, you may graduate to the full liquid diet. This stage is critical because you cannot sustain yourself on apple juice and broth forever. You need protein to heal.

Liquid Meal Replacements and Protein Shakes
This is the phase where products like Ensure or Boost become valuable. These liquid meal replacements are formulated to provide complete nutrition.
- Selection Criteria: Look for “Original” or “High Protein” formulas.
- Avoid: Do not buy “High Fiber” or “digestive health” versions yet. Fiber is still the enemy at this stage.
- Usage: Sip these slowly. Drinking a high-calorie shake too fast can cause nausea in a sensitive stomach.
Smooth Dairy and Strained Soups
You can now introduce dairy or plant-based alternatives. Milk, soy milk, and almond milk are excellent sources of calcium and protein.
- Cream Soups: You can eat cream of mushroom, tomato, or chicken soup, but there is a catch. You must strain out every solid piece of mushroom, tomato, or meat. You are consuming the broth and the cream base only.
- Yogurt: Plain, smooth yogurt is allowed. Avoid varieties with fruit chunks, seeds, or granola mixed in. Greek yogurt is excellent for its high protein content, provided it is perfectly smooth.
Vegetable Juices for Nutrient Intake
Vegetable juices like V8 can be introduced now, but they must be smooth. If you are juicing at home, you must use a high-quality strainer or cheesecloth to remove all pulp. This provides vitamins without the insoluble fiber that bulks up the stool.
Navigating Common Triggers and “Forbidden” Drinks
Even within the realm of liquids, some choices can worsen your condition. A liquid diet for diverticulitis is not just about texture. It is about chemical composition.

The Caffeine and Coffee Debate
Many patients ask, “Can I drink coffee during a flare?” Technically, black coffee is a clear liquid. However, caffeine is a stimulant. It stimulates the colon to contract.
If your goal is bowel rest, caffeine works against you. It can induce spasms in the sigmoid colon, leading to sharp cramping. It is highly advisable to switch to decaf or herbal teas during the acute phase. If you must have caffeine to avoid withdrawal headaches, limit it to a small cup and ensure it is not on an empty stomach.
Alcohol Risks and Antibiotics
Alcohol is strictly forbidden during a diverticulitis flare up diet. First, alcohol causes dehydration. Second, and more importantly, diverticulitis is often treated with antibiotics like Flagyl (metronidazole) or Cipro (ciprofloxacin).
Combining alcohol with Flagyl can cause severe reactions, including violent vomiting and rapid heart rate. Even without antibiotics, alcohol irritates the lining of the stomach and intestine, counteracting the healing process.
Carbonation and Gas Pressure
Avoid soda, sparkling water, and carbonated energy drinks. Carbonation introduces gas into the digestive tract. In a healthy gut, this is a minor annoyance. In a gut affected by colon inflammation, trapped gas can exert pressure on the diverticula, mimicking the pain of the infection and making it difficult to judge if you are healing.
The “Seeds and Nuts” Myth vs. Reality
For decades, doctors told patients to avoid seeds, nuts, and popcorn forever. Recent research published in JAMA (Journal of the American Medical Association) has largely debunked this as a cause of diverticulitis.
However, context is vital. While seeds may not cause the initial formation of diverticula, you absolutely must avoid them during an active flare. During the liquid and low-residue phases, a stray sesame seed or nut fragment can irritate the already inflamed tissue. The “no seeds” rule applies strictly during the recovery phase.
Essential Shopping List for Diverticulitis Care
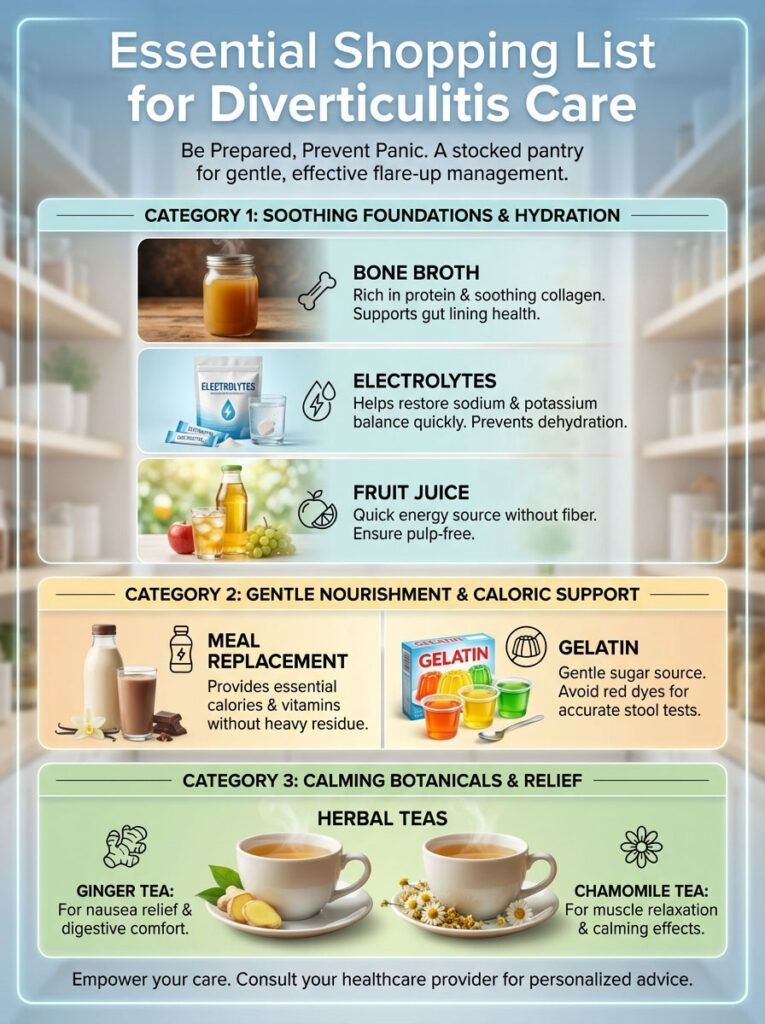
Being prepared prevents panic. If you have a history of diverticulosis, keeping a “Go-Bag” or specific pantry items on hand can make the onset of a flare much less stressful.
| Category | Recommended US Brands/Types | Why It Helps |
| Bone Broth | Pacific Foods, Kettle & Fire (Chicken/Beef) | Rich in protein and soothing collagen for the gut. |
| Electrolytes | Pedialyte, Gatorade Zero, Liquid I.V. | Rapidly restores sodium and potassium balance. |
| Meal Replacement | Ensure Clear, Boost Breeze | Provides calories and vitamins without fat or heavy residue. |
| Gelatin | Jell-O (Lemon, Lime, Orange) | Gentle sugar source. Avoid red dyes if seeing a doctor for stool tests. |
| Herbal Teas | Traditional Medicinals (Ginger, Chamomile) | Ginger helps nausea; Chamomile relaxes smooth muscle spasms. |
| Fruit Juice | Mott’s Apple Juice, Ocean Spray White Cranberry | Provides quick energy (glucose) without fiber. |
Determining When to End the Liquid Diet
Knowing when to stop the liquid diet for diverticulitis is just as important as starting it. Prolonged restriction of calories and protein can lead to fatigue and muscle wasting.
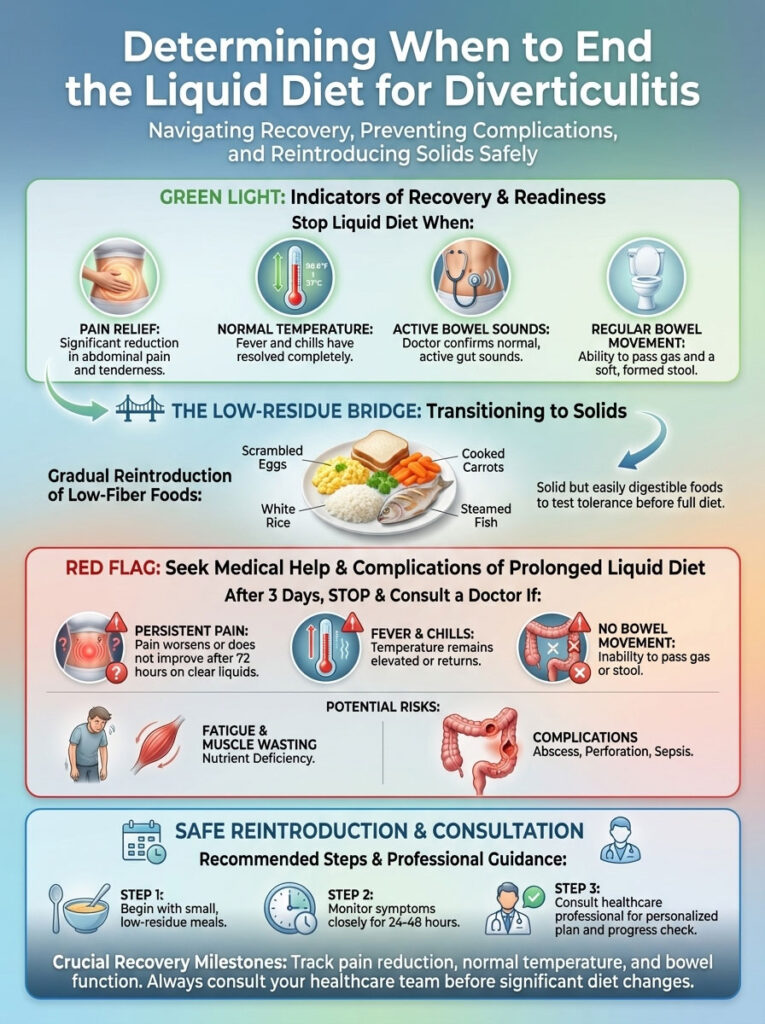
Clinical Indicators of Recovery
You should look for specific signs before chewing solid food again:
- Pain Reduction: The sharp, stabbing pain has subsided to a mild discomfort or is gone entirely.
- No Fever: Your body temperature has returned to normal without medication.
- Appetite Return: You actually feel hungry, not just empty.
- Bowel Function: You may not have a normal movement yet due to lack of bulk, but you are passing gas easily without pain.
The Low-Residue Bridge
You do not jump from liquids to a salad. You must cross the “Low-Residue Bridge.” This involves eating foods that are solid but easily digested.
- Scrambled eggs.
- White toast (no seeds, no whole wheat).
- White rice.
- Canned fruit (no skin).
- Poached chicken.
When to Seek Medical Help
If you have been on a clear liquid diet for 3 days and your pain is unchanged or worsening, this is a red flag. It suggests that oral antibiotics and diet alone may not be enough. You may have a complication like an abscess or a perforation. In this scenario, you must seek professional medical attention immediately.
Real-World Recovery Scenarios
To illustrate how this works, consider two common profiles.
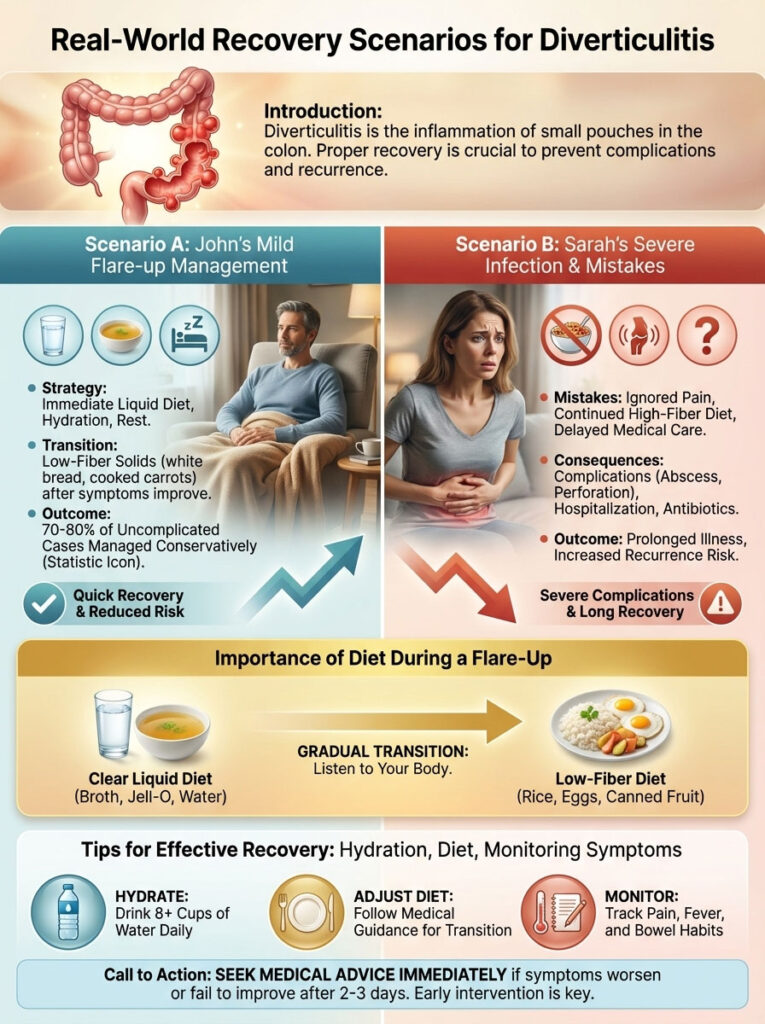
Scenario A: Mild Flare at Home
“John,” a 55-year-old male, feels the familiar twinge in his lower left abdomen. He immediately stops eating dinner and switches to water and broth. The next morning, he buys apple juice and Jell-O. He adheres to the diverticulitis flare up diet for 48 hours. By day 3, the pain is gone. He eats scrambled eggs for breakfast and plain pasta for dinner. He avoided the ER entirely.
Scenario B: Severe Infection
“Sarah,” 42, ignores the pain and eats a high-fiber salad, thinking it will help “move things along.” The fiber causes intense contractions. Her pain spikes to an 8/10, and she develops a fever of 102°F. She requires hospitalization for IV antibiotics and strict bowel rest.
These instances highlight that early intervention with the correct what to drink for diverticulitis pain strategy is the single most effective tool a patient has. American Family Physician data suggests that 70-80% of uncomplicated cases can be successfully managed conservatively like John, provided the diet is started immediately.
Summary & Key Takeaways
Recovering from diverticulitis is a test of patience. The liquid diet for diverticulitis is your primary tool for reducing inflammation and allowing the colon to heal itself.

- Act Fast: Switch to clear liquids the moment you suspect a flare.
- Stay Hydrated: Drink 8–12 cups of water, broth, and electrolyte drinks daily.
- Be Patient: Do not rush the transition to full liquids or solids.
- Monitor Symptoms: If fever or pain persists past 72 hours, consult a doctor.
By respecting the biology of your colon and providing it with the rest it requires, you can often manage this painful condition from the comfort of your home.
Frequently Asked Questions (FAQ)
How long can I safely stay on a liquid diet for diverticulitis?
Most gastroenterologists recommend staying on a clear liquid diet for no more than 2 to 3 days (48–72 hours). If symptoms do not improve within this window, you should contact your doctor. Prolonged liquid diets without medical supervision can lead to malnutrition.
Is bone broth better than regular chicken broth for diverticulitis?
Yes, bone broth is generally preferred. It contains higher levels of protein and collagen compared to standard stock. The amino acids in bone broth, such as glutamine, may help support the repair of the intestinal lining during diverticulitis recovery.
Can I drink coffee or tea during a diverticulitis flare-up?
Tea is generally safe, especially herbal varieties like chamomile. Coffee is controversial; while it is a clear liquid, the caffeine can stimulate the colon and cause spasms. It is best to avoid coffee or switch to decaf during the acute pain phase.
Which protein shakes are safe for diverticulitis recovery?
During the “Full Liquid” stage (Stage 2), you can drink shakes like Ensure Original, Boost, or Glucerna. Ensure you choose the standard versions, not the “High Fiber” varieties, as fiber can irritate the sigmoid colon while it is still healing.
Does apple cider vinegar help with diverticulitis pain?
There is no clinical evidence that apple cider vinegar treats diverticulitis. In fact, its high acidity might irritate an already sensitive stomach. It is better to stick to neutral, soothing liquids like broth and water.
Can I eat applesauce on a clear liquid diet?
No. Applesauce is considered a solid or puree, not a clear liquid. It fits into the “soft food” or low-residue diet phase, which comes after you have successfully tolerated full liquids.
Is pulp-free orange juice safe for my colon?
Yes, but with caution. It must be 100% pulp-free. However, the acidity of orange juice can sometimes cause heartburn or gastric distress. Apple or white grape juice is typically gentler on the stomach during a diverticulitis flare up diet.
What usually triggers a diverticulitis flare-up?
While diet plays a role, the exact trigger is often unclear. It involves high pressure in the colon causing a pouch to tear or become infected. Chronic constipation, low fiber intake over years, and obesity are risk factors, but a specific food event doesn’t always cause the attack immediately.
Can I drink alcohol while recovering from diverticulitis?
No. Alcohol should be avoided completely. It causes dehydration and can interact dangerously with antibiotics often prescribed for diverticulitis, such as metronidazole (Flagyl), causing severe nausea and vomiting.
What is the difference between diverticulosis and diverticulitis diets?
The diets are opposites. Diverticulosis (the chronic condition) requires a high-fiber diet to prevent issues. Diverticulitis (the acute infection) requires a low-fiber or liquid diet to treat the immediate inflammation.
Are eggs considered part of a liquid diet?
No. Eggs are a solid food. However, they are one of the first foods recommended when you transition off the liquid diet because they are soft, high in protein, and very low in residue.
Should I take fiber supplements like Metamucil during a flare?
Absolutely not. You must stop all fiber supplements during an acute attack. Adding bulk to an inflamed colon will increase pressure and pain. Resume fiber supplements only after you have fully recovered, with your doctor’s approval.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK). “Definition & Facts for Diverticular Disease.”
- American Gastroenterological Association (AGA). “Management of Acute Diverticulitis.”
- Peery AF, et al. “Burden of Gastrointestinal Disease in the United States.” Gastroenterology.
- Strate LL, et al. “Nut, Corn, and Popcorn Consumption and the Incidence of Diverticular Disease.” JAMA.
- American Family Physician. “Diagnosis and Management of Acute Diverticulitis.”