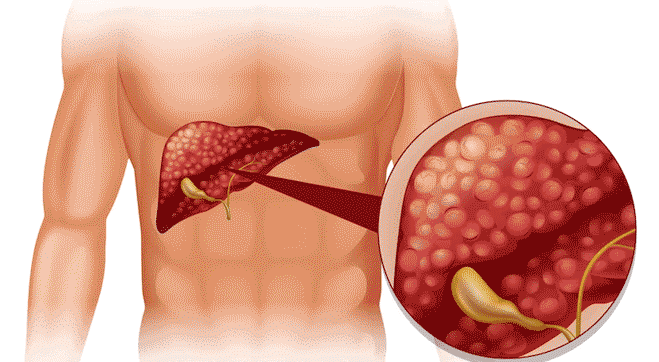
Liver- An Indispensable Organ
One of the largest organs in the body, the liver supports almost every other organ in the body. It
consists of two lobes connected by the falciform ligament which anchors it to the diaphragm. It is
a part of a complex processing system which ensures that all parts of the body receive energy and
nutrients in sufficient amounts. It is also involved in both, the removal of waste produced by the body
and in neutralizing the nutrients and drugs in our body.