A low fiber diet for diverticulitis is a temporary nutritional protocol designed to treat inflammation in the colon. Also known as a low-residue diet, it restricts daily fiber intake to 10–15 grams to decrease stool volume and bowel frequency. This provides “mechanical rest” for the sigmoid colon. Safe foods include refined grains like white rice and white bread, tender proteins such as eggs and poultry, and well-cooked vegetables without skins or seeds. This diet bridges the gap between liquid nutrition and a return to normal high-fiber eating.
Table of Contents
The sharp and sudden pain in the lower left abdomen is often the first warning sign. For the millions of Americans navigating a diagnosis of diverticulitis, the immediate aftermath brings a wave of anxiety regarding food choices. The very diet that doctors recommend for preventing gut issues—high fiber, raw salads, whole grains—suddenly becomes the enemy. When the colon is inflamed or infected, the rules of nutrition flip upside down. You are no longer eating for long-term prevention. You are eating for immediate survival and recovery.
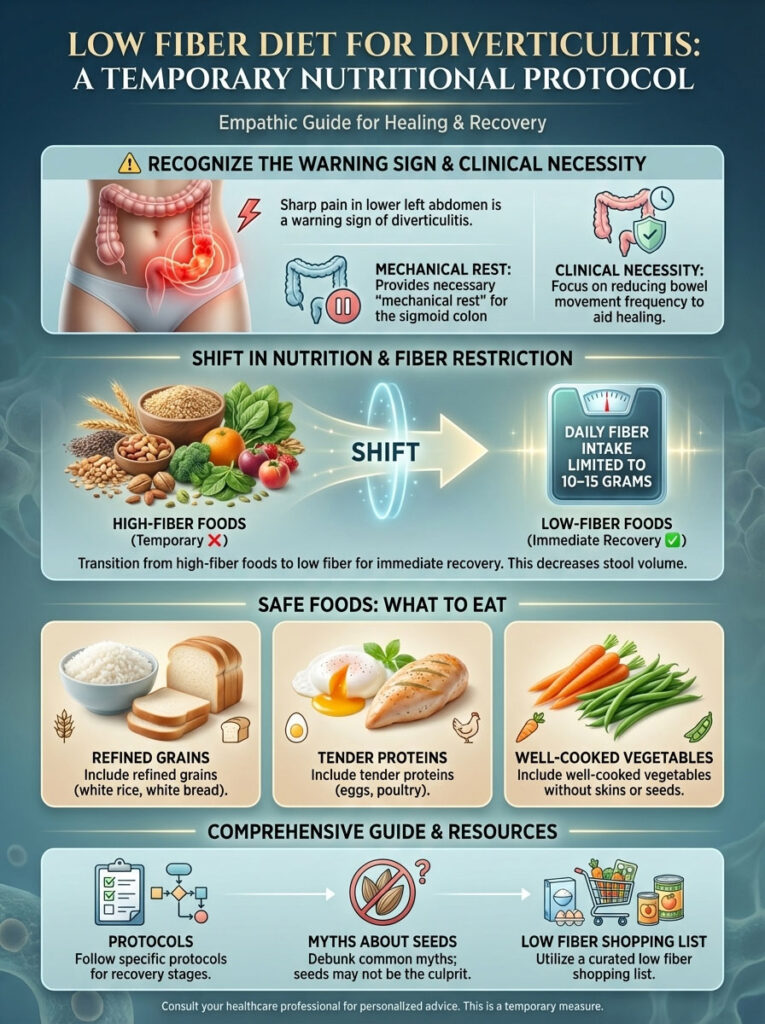
Managing this condition requires a strategic and temporary shift to low fiber foods for diverticulitis. This approach is not about unhealthy eating. It is about clinical necessity. The goal is to reduce the volume and frequency of bowel movements to allow the sigmoid colon time to heal without the irritation caused by bulky waste. This guide bridges the gap between the initial clear liquid diet prescribed in the emergency room and the return to normal eating. We will cover the specific diverticulitis diet protocols, bust outdated myths about seeds, and provide a comprehensive low fiber shopping list approved by modern gastroenterology standards.
Understanding Diverticulosis vs. Diverticulitis in Recovery
To effectively manage your diet, you must understand the biological difference between the two stages of diverticular disease. Confusion between these terms often leads to painful dietary errors.
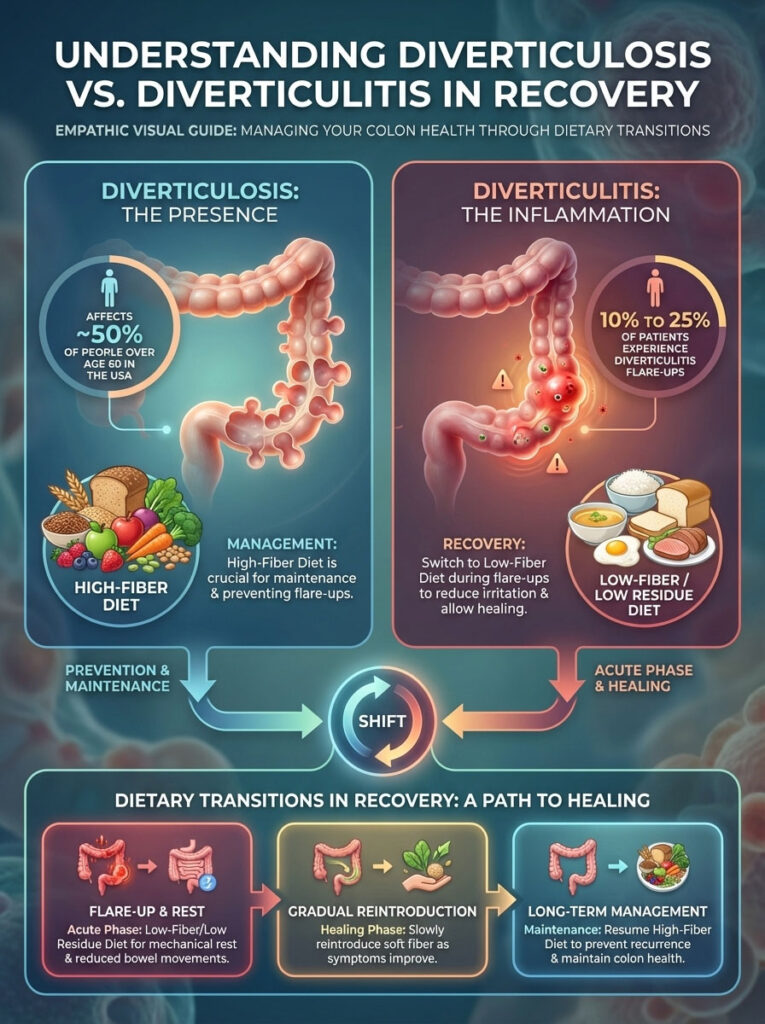
The Condition of Diverticulosis
Diverticulosis is the chronic condition of having small pouches, known as diverticula, bulging outward through weak spots in the colon wall. It affects approximately 50% of people over age 60 in the USA. In this phase, a high-fiber diet is essential. Fiber keeps stool soft and bulky, preventing the high pressure that forces these pouches to form in the first place.
The Infection of Diverticulitis
Diverticulitis occurs when those pouches become inflamed or infected. This can be caused by a micro-perforation or bacterial overgrowth. Statistics indicate that 10% to 25% of individuals with diverticulosis will eventually experience a diverticulitis flare-up. During this acute phase, you must stop the high-fiber regimen immediately and switch to low fiber foods for diverticulitis. Treating the infection requires minimizing bowel contractions. High-fiber foods during a flare-up act like sandpaper on an open wound. The low residue diet removes abrasive elements, allowing the tissue to repair itself.
The Science Behind the Low Residue Diet and Bowel Rest
The primary objective of eating low fiber foods for diverticulitis is to achieve what gastroenterologists call “mechanical rest.” This is a critical concept for recovery.
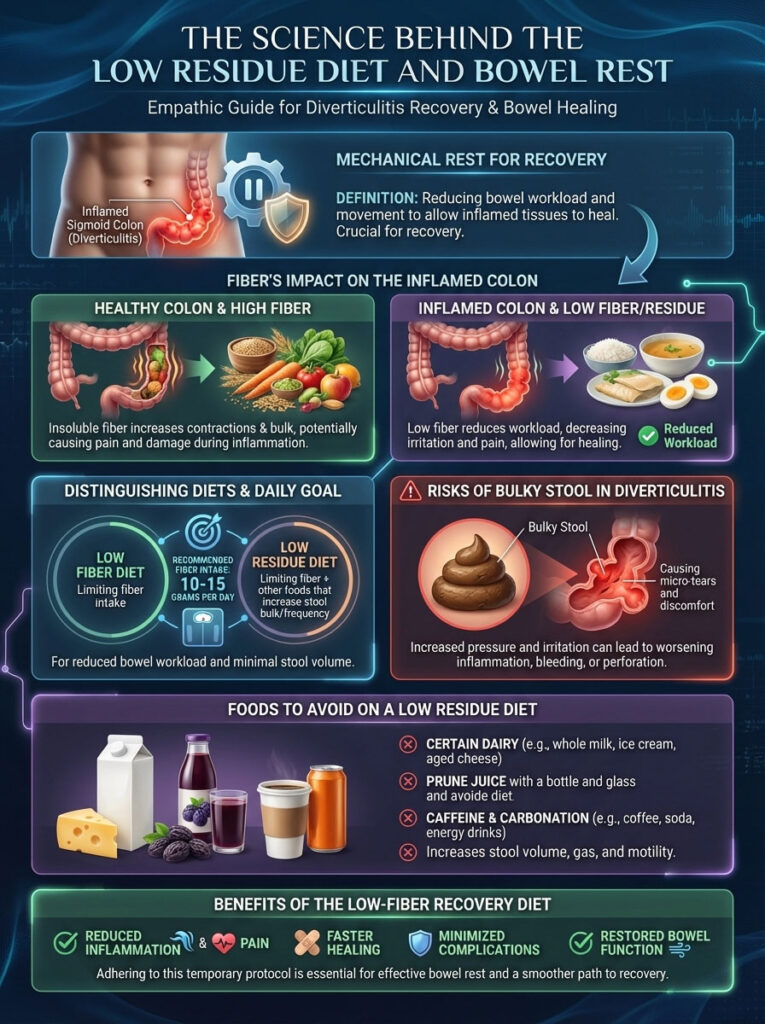
How Fiber Affects an Inflamed Sigmoid Colon
Fiber, particularly insoluble fiber found in wheat bran, kale, and vegetable skins, is indigestible. It passes through the stomach and small intestine relatively intact. When it reaches the colon, it adds significant bulk to the stool and draws in water. In a healthy gut, this stimulates peristalsis, the rhythmic contraction of the bowel muscles.
However, when the sigmoid colon is inflamed, these contractions cause intense pain. The pressure from bulky stool can threaten to worsen the micro-perforations in the diverticula. By restricting fiber intake to 10–15 grams per day, you reduce the physical workload of the bowel. The stool becomes smaller and passes with less muscular effort, reducing the risk of abscess formation or rupture.
The Low Residue Distinction
You may hear your doctor use the terms “low fiber” and “low residue” interchangeably, but there is a medical nuance. A low fiber diet strictly limits fiber grams. A low residue diet is more restrictive. It limits fiber but also restricts foods that stimulate bowel activity or leave metabolic residue, such as dairy (for some), prune juice, and caffeine. For the purpose of this guide, we focus on the standard medical definition of a low-fiber recovery diet which naturally lowers residue.
Comprehensive Low Fiber Shopping List for Diverticulitis
Navigating the grocery store during a flare-up can be overwhelming. Reading nutrition labels for fiber content is exhausting when you are in pain. This low fiber shopping list is categorized by aisle to make your trip efficient and safe.

Refined Grains and Bread Options for Diverticulitis
When selecting low fiber foods for diverticulitis, you must look for “refined” on the label. The refining process removes the bran and germ which contain the fiber.
- White Bread and Rolls: Traditional white bread, Italian bread, and potato bread are staples. Sourdough is an excellent choice; the fermentation process pre-digests some of the starches, making it easier on the gut.
- Refined Bagels and Muffins: Plain bagels, English muffins, and croissants are safe. Avoid anything with sesame or poppy seeds on top.
- White Tortillas: Flour tortillas are safe. Corn tortillas are high in fiber and should be avoided.
- Why This Works: These refined grains are digested almost entirely in the upper gastrointestinal tract. By the time the remnants reach the colon, there is very little waste left to irritate the diverticula.
Safe Cereal and Breakfast Foods
Breakfast is often the hardest meal to adjust, as healthy habits usually dictate oatmeal or bran flakes. You must temporarily reverse this habit.
- Hot Cereals: Cream of Wheat, Cream of Rice, and grits are safe. They provide warmth and easy calories.
- Cold Cereals: Look for corn-based or rice-based cereals with less than 1 gram of fiber per serving. Examples include Corn Flakes, Rice Krispies, and Special K.
- Pancakes and Waffles: Plain pancakes made with white flour are acceptable. Avoid whole grain or buckwheat mixes.
Low Fiber Produce Selection and Preparation
The produce section is usually the “danger zone” for a low residue diet, but you do not need to eliminate plants entirely. You simply need to change how you select and prepare them. The rule is: Peel it, seed it, cook it.
- Safe Vegetables: Carrots, green beans, asparagus tips, beets, pumpkin, and zucchini.
- Mandatory Preparation: All vegetables must be cooked until soft (fork-tender) or pureed. Canned vegetables are excellent options because the canning process breaks down the fibrous cell walls.
- Potatoes: White or sweet potatoes are excellent energy sources, but they must be peeled. The skin is pure insoluble fiber.
- Safe Fruits: Ripe bananas (speckled skin is best), cantaloupe, honeydew melon, watermelon, and avocado (in small amounts).
- Canned Fruits: Canned peaches, pears, and mandarin oranges are safe if they are peeled.
- Avoid: Raw salads, broccoli, cauliflower, Brussels sprouts, corn, peas, berries with seeds (strawberries/raspberries), and dried fruits like raisins or dates.
Lean Proteins and Meats for Colon Recovery
Animal proteins are naturally free of fiber, making them a staple of the diverticulitis flare up foods list. However, high-fat or tough meats can slow digestion and cause spasms.
- Poultry: Skinless chicken breast and turkey breast are the safest options.
- Fish: White fish like cod, tilapia, halibut, and flounder are easy to digest. Salmon is also acceptable if not fried.
- Eggs: Eggs are the gold standard for recovery. They are soft, nutrient-dense, and contain zero fiber. Scrambled or poached eggs are gentle on the stomach.
- Tofu: For vegetarians, firm or silken tofu is a perfect low-fiber protein source.
- Smooth Nut Butters: Creamy peanut butter or almond butter provides calories and healthy fats. You must avoid crunchy varieties.
Safe Dairy and Pantry Staples
Stocking your pantry with the right low fiber foods for diverticulitis ensures you always have a safe meal ready.
- Dairy: Milk, Greek yogurt (vanilla or plain, no fruit chunks), cottage cheese, hard cheeses (Cheddar, Swiss, Parmesan), and butter. Dairy has no fiber.
- Lactose Caution: Even if you are not usually lactose intolerant, a gut infection can cause temporary sensitivity. Consider lactose-free milk or hard cheeses which are naturally lower in lactose.
- Pasta and Rice: White rice (Jasmine or Basmati) and regular white pasta are essential calorie sources.
- Condiments: Mayonnaise, mustard, soy sauce, ketchup, and honey are all safe.
- Snacks: Saltine crackers, vanilla wafers, pretzels, and gelatin (Jell-O).
Comparison Table: Low Fiber vs. High Fiber Foods
It is vital to distinguish between what helps you recover and what prevents future attacks. This table clarifies the difference between low fiber foods for diverticulitis (Recovery Mode) and high fiber foods (Prevention Mode).
| Food Category | Safe for Flare (Low Fiber/Residue) | Avoid During Flare (High Fiber) |
| Grains | White rice, white pasta, Cream of Wheat, white bread | Brown rice, quinoa, oatmeal, bran cereal, whole wheat bread |
| Fruits | Canned peaches (peeled), bananas, melon, applesauce | Berries (seeds), raw apples with skin, pears with skin, dried fruit |
| Vegetables | Well-cooked carrots, spinach (pureed), peeled potatoes | Raw salads, broccoli, cauliflower, corn, cabbage, kale |
| Proteins | Eggs, tender chicken, tofu, smooth nut butter | Legumes, lentils, kidney beans, crunchy nut butter |
| Dairy | Milk, cheese, smooth yogurt, cottage cheese | Yogurt with fruit chunks, granola, or added fiber |
Data Source: USDA FoodData Central and ACG Clinical Guidelines.
Cooking and Meal Preparation for Recovery
Knowing what to buy is only half the battle. How you cook your food is equally important for a low residue diet.

Gentle Cooking Techniques
Frying food adds excess oil which can trigger the gastrocolic reflex, causing the colon to contract vigorously. This is painful during a flare-up.
- Poaching: Cooking chicken or fish in water or broth keeps the meat tender and digestible.
- Steaming: This softens the fibers in vegetables like carrots and green beans without adding fat.
- Baking/Roasting: Wrapping food in foil while baking helps retain moisture.
Seasoning and Flavoring Without Irritation
Food on a diverticulitis diet does not have to be bland. However, you must be careful with spices.
- Safe Herbs: Salt, parsley, dill, basil, and thyme are generally well tolerated.
- Spices to Avoid: Chili powder, cayenne pepper, hot paprika, and curry powder. Capsaicin in hot peppers can irritate the mucosal lining of the gut.
- Garlic and Onion: These are high in FODMAPs (fermentable carbohydrates). While they don’t have fiber, they can cause gas. It is safer to use garlic-infused oil or onion powder in small amounts rather than whole cloves during the acute phase.
The Recovery Timeline and Phases
Recovering from a flare-up is not an overnight process. It requires a phased approach to reintroducing food. Jumping straight into a standard diet can cause an immediate relapse.

Phase 1: The Clear Liquid Diet Protocol
Immediately following diagnosis or the onset of severe pain, strict bowel rest is required. This phase is calorie-deficient and should not last more than a few days without medical supervision.
- Purpose: Total bowel rest. Hydration is the priority.
- Allowed Items: Bone broth, vegetable broth, herbal tea, apple juice (no pulp), white grape juice, gelatin (Jell-O), clear soda (ginger ale), water, and ice pops.
- Red Dye Warning: Some doctors advise avoiding red or purple dyes in Jell-O or drinks, as the color can be mistaken for blood in stool or during diagnostic imaging.
- Duration: Typically 1 to 3 days.
Phase 2: The Low Fiber “Soft” Diet
Once the sharp pain subsides and you feel hungry, you move to the core diverticulitis diet.
- Goal: Fiber intake per day should be restricted to 10–15 grams.
- Strategy: Eat small, frequent meals rather than three large ones. This prevents the stomach from becoming too full and stimulating a massive bowel movement.
- Duration: This phase usually lasts 2 to 4 weeks depending on the severity of the infection. You should wait until you are completely symptom-free before moving to the next phase.
Phase 3: The Transition Phase
This is the most critical and dangerous phase. Many patients feel better and immediately eat a salad, causing a setback.
- Goal: Gradual reintroduction of fiber.
- Strategy: Add 3 to 5 grams of fiber back into your diet every 3 days.
- The Order Matters: Start with soluble fiber before introducing insoluble fiber.
Comparison Table: Soluble vs. Insoluble Fiber for Transition
Understanding the two types of fiber is the key to mastering the transition from the diverticulitis diet back to normal eating.
| Feature | Soluble Fiber | Insoluble Fiber |
| Function | Dissolves in water; forms a gel-like substance. | Does not dissolve; adds bulk and “roughage” to stool. |
| Effect on Gut | Slows digestion; soothes the intestinal lining. | Speeds up passage; “scrubs” the colon wall. |
| Role in Diverticulitis | Safer to introduce first during transition. | The main trigger during a flare; avoid until fully healed. |
| Best Time to Eat | Early Transition Phase (Week 4). | Late Recovery / Prevention Phase. |
| Food Examples | Oats, flesh of fruits, barley, root vegetables. | Wheat bran, potato skins, seeds, corn, nuts. |
Note: Most plant foods contain a mix of both types of fiber, but usually one dominates. Focus on the texture: if it turns to mush in water (oats), it is soluble. If it stays tough (bran), it is insoluble.
Detailed Meal Plans and Recipes
Decision fatigue is real when you are sick. Use this meal plan to ensure you stick to low fiber foods for diverticulitis without overthinking.
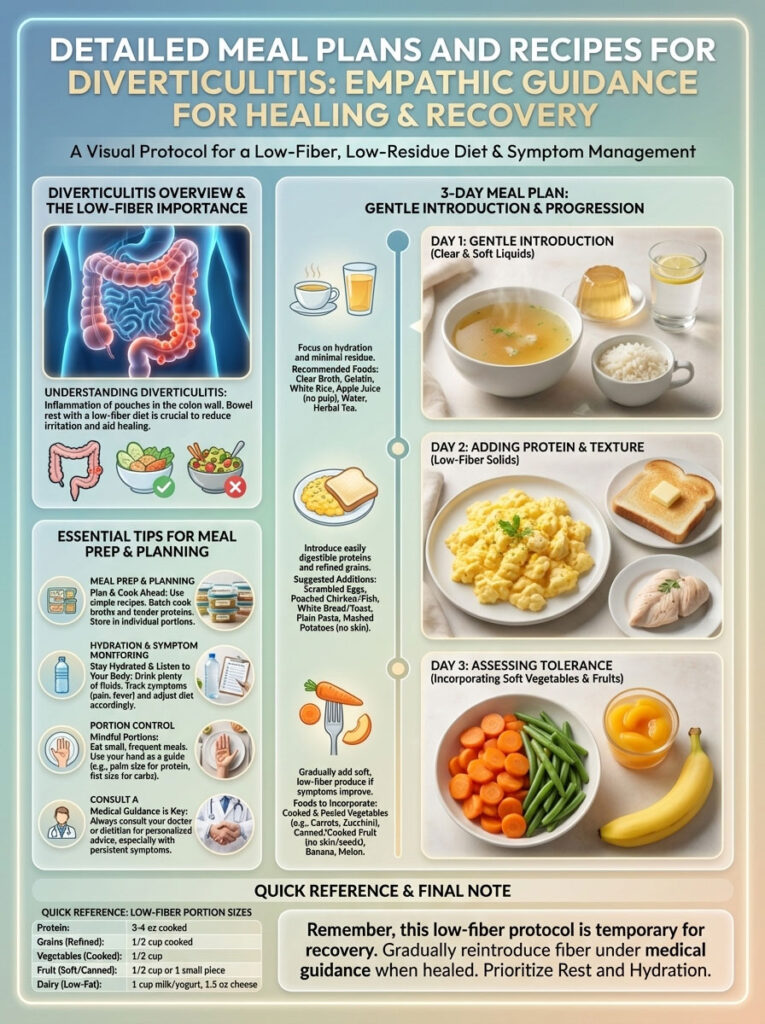
Day 1: Gentle Introduction
- Breakfast: Two scrambled eggs, one slice of white sourdough toast with butter, weak tea.
- Snack: A small cup of smooth applesauce.
- Lunch: Chicken noodle soup. Use white pasta and peel the carrots. Eat with saltine crackers.
- Dinner: Baked white fish (cod) seasoned with salt, lemon, and dill. Serve with a side of steamed white rice.
- Dessert: A vanilla popsicle.
Day 2: Adding Protein and Texture
- Breakfast: Cream of Wheat made with milk or soy milk, sweetened with a drizzle of honey.
- Snack: Vanilla Greek yogurt (smooth, no fruit on the bottom).
- Lunch: Turkey sandwich. Use white bread and thinly sliced turkey breast. Add mild mustard or mayonnaise. No lettuce or tomato.
- Dinner: Lean ground beef patty (grilled or baked). Serve with mashed potatoes (peeled, mashed with milk and butter) and well-cooked green beans.
Day 3: Assessing Tolerance
- Breakfast: Rice Chex cereal with milk and half a ripe banana.
- Snack: A slice of cheddar cheese and white crackers.
- Lunch: Tuna salad made with light mayo. Serve on a soft white roll or with pretzels.
- Dinner: Roast chicken breast. Serve with glazed cooked carrots and a small portion of white pasta tossed with olive oil and parmesan cheese.
Nutritional Risks and Supplementation Strategies
Adhering to a low residue diet for an extended period creates a nutritional gap. Whole grains and vegetables are our primary sources of vitamins and minerals. Relying on white bread and rice for weeks can lead to deficiencies if not managed.

Addressing the Micronutrient Gap
The most common deficits seen in patients on long-term restrictive diets include Magnesium, Vitamin B12, and Iron.
- Magnesium: Usually found in leafy greens and nuts, which you are avoiding. Symptoms of deficiency include muscle cramps and fatigue.
- Vitamin C: Found in citrus and raw veg. You can mitigate this by drinking pulp-free orange juice or vitamin-fortified apple juice.
- Strategy: If your doctor anticipates you will be on low fiber foods for diverticulitis for more than two weeks, ask about a liquid multivitamin. Liquid forms are easier to absorb and do not require the stomach to break down a hard pill.
Probiotics and Gut Health Restoration
Antibiotics prescribed for diverticulitis recovery kill both the bad bacteria causing the infection and the good bacteria in your gut. This can lead to antibiotic-associated diarrhea or Clostridioides difficile (C. diff) infection.
- The Solution: Probiotics can help restore the microbiome. Strains like Lactobacillus casei and Saccharomyces boulardii have shown promise in reducing recurrence and managing symptoms.
- Food Source: Yogurts with “live active cultures” are the safest food source during recovery.
- Supplementation: Consult your gastroenterologist before adding a probiotic capsule. Some supplements contain prebiotics (fiber that feeds bacteria) like inulin or chicory root, which might cause excessive gas and pain during a flare.
Long-Term Prevention and Lifestyle Strategy
Once you have successfully navigated the low fiber foods for diverticulitis phase and reintroduced fiber, the goal shifts to prevention. You never want to be on a low fiber diet permanently.

Increasing Fiber Safely
The long-term goal for preventing diverticulitis recurrence is a high-fiber diet (25 to 35 grams daily). Fiber keeps the stool soft and bulky, reducing the colonic pressure that creates diverticula.
- Hydration is Mandatory: As you increase fiber, you must increase water intake. Fiber without water creates a blockage, which is dangerous for someone with diverticular disease. Aim for at least 64 ounces of water daily, more if you are active.
- Chewing Thoroughly: Digestion begins in the mouth. Chewing food until it is a paste reduces the work your colon has to do.
- Regular Exercise: Physical activity stimulates normal bowel function and reduces pressure in the colon.
The Truth About Nuts, Seeds, and Popcorn
For decades, doctors advised avoiding nuts, corn, popcorn, and seeds. This theory has been rigorously tested and largely debunked. The American College of Gastroenterology (ACG) now states that there is no evidence linking nut or seed consumption to diverticulitis attacks. In fact, some studies suggest that people who eat nuts and popcorn have lower rates of diverticulitis because these foods are high in fiber. Once you are fully healed, these foods should be part of your healthy diet.
Frequently Asked Questions (FAQs)
How long should I stay on a low fiber diet for diverticulitis?
You should typically remain on low fiber foods for diverticulitis until all symptoms—such as abdominal pain, fever, and digestive changes—have completely resolved. This usually takes 2 to 4 weeks. Always consult your doctor before reintroducing high-fiber foods to ensure the infection has cleared.
Is coffee allowed during a diverticulitis flare-up?
Coffee is technically a low-residue liquid, so it is often allowed on the diverticulitis diet. However, caffeine is a bowel stimulant that can increase colonic motility, potentially causing cramping. Decaffeinated coffee is a safer option, but stick to water or herbal tea if you experience discomfort.
Can I eat peanut butter with diverticulitis?
Yes, smooth peanut butter is safe and a good source of protein and healthy fats. You must avoid crunchy or extra-crunchy peanut butter during the acute phase, as the nut fragments are insoluble fiber that can irritate the inflamed diverticula.
Are eggs good for diverticulitis recovery?
Absolutely. Eggs are one of the best foods for diverticulitis recovery. They provide high-quality protein, are soft and easy to digest, and contain zero fiber. They can be prepared scrambled, poached, or boiled.
Why do doctors recommend white bread instead of whole wheat?
During a flare, your goal is bowel rest. Whole wheat bread is rich in insoluble fiber, which adds bulk to stool and forces the colon to work harder. White bread is refined, meaning the fiber has been removed, making it one of the safest low fiber foods for diverticulitis.
What vegetables are safe to eat?
Vegetables are safe if they are canned or well-cooked and have no skins or seeds. Excellent choices include carrots, green beans, asparagus tips, and peeled potatoes. You should avoid gas-producing or fibrous vegetables like broccoli, cauliflower, and corn.
Can I drink milk or eat cheese?
Yes, unless you are lactose intolerant. Dairy products like milk, cheese, and yogurt contain no fiber and are generally safe. However, avoid yogurts that contain added fruit chunks, berries, or granola, as these add fiber.
Is oatmeal considered a low fiber food?
No, oatmeal is a whole grain and contains significant fiber. During the acute phase of a flare, it is better to choose Cream of Wheat, Cream of Rice, or corn-based cereals which have lower residue.
What sweet snacks can I have?
Safe sweet snacks on a low residue diet include gelatin (Jell-O), popsicles (without fruit pulp), vanilla wafers, plain sponge cake, custard, or hard candies. Chocolate is allowed in moderation if it does not contain nuts or dried fruit.
Do I need to avoid seeds and nuts forever?
No. Current clinical guidelines from the American College of Gastroenterology (ACG) indicate that once you have fully recovered, you do not need to permanently avoid seeds, nuts, or popcorn. They do not increase the risk of recurrence for the majority of patients.
What is the difference between diverticulosis and diverticulitis?
Diverticulosis is the presence of small pouches in the colon wall, which requires a high-fiber diet for management. Diverticulitis is the infection of those pouches, which requires a temporary low-fiber diet for healing.
Can stress cause a diverticulitis flare-up?
While stress does not cause the infection directly, it affects the gut-brain axis. High stress can worsen inflammation and gut motility issues, which may trigger symptoms or make a flare-up feel more painful.
Disclaimer
The information provided in this article is for educational purposes only and does not constitute medical advice, diagnosis, or treatment. Always seek the advice of your physician or other qualified health provider with any questions you may have regarding a medical condition. Never disregard professional medical advice or delay in seeking it because of something you have read in this article.
References
- Peery, A. F., et al. (2021). “Management of Acute Diverticulitis.” American Journal of Gastroenterology.
- Strate, L. L., & Morris, A. M. (2019). “Epidemiology, Pathophysiology, and Treatment of Diverticulitis.” Gastroenterology.
- Mayo Clinic Staff. “Diverticulitis Diet.” Mayo Clinic Guidelines.
- USDA FoodData Central. “Fiber Content of Common Foods.”








