I see her in my clinic almost every day. She is 47 years old, exhausted, and sitting on the exam table with a list of symptoms that she cannot make sense of. She has gained ten pounds around her midsection despite eating salads. She feels “mentally fuzzy” at work. She wakes up sweating at 3 AM. Her primary care physician ran a basic blood panel and told her everything was “normal.” She feels anything but normal. This is the classic clinical presentation of the Menopause vs. Hypothyroidism dilemma.
Table of Contents
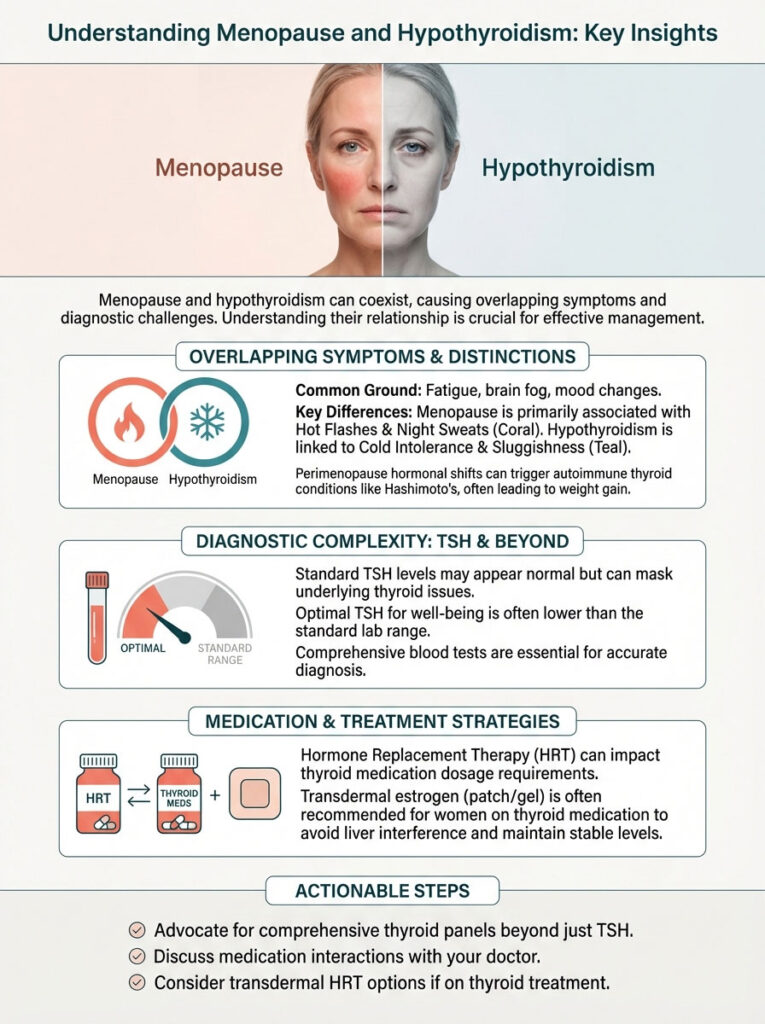
As a gynecologist and certified menopause practitioner, I spend a significant portion of my clinical time untangling these two conditions. They are the “Great Mimics” of women’s health. Both involve major hormonal shifts. Both dismantle your metabolism. Most frustratingly, both often happen at the exact same time.
The goal of this article is to move beyond surface-level symptom lists. We are going to look at the specific interaction between your ovarian function and your thyroid health. You need to understand the biology so you can finally advocate for the right testing and treatment.
Quick Clinical Distinction
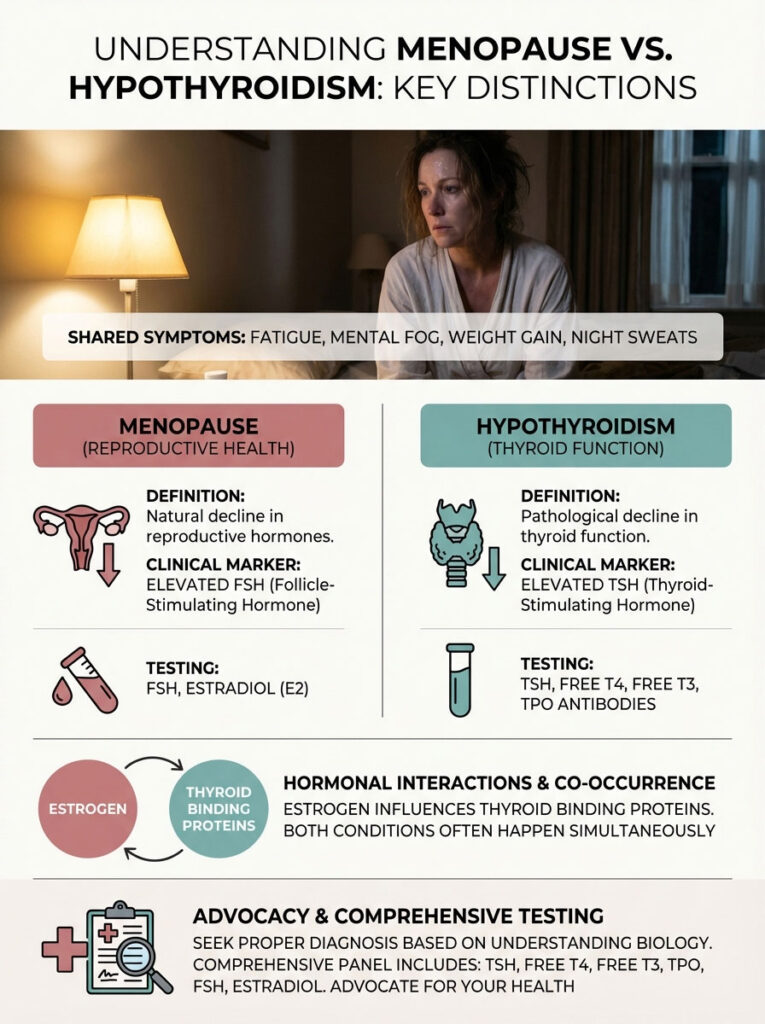
Menopause is a natural decline in reproductive hormones characterized by elevated FSH and vasomotor symptoms like heat flashes. Hypothyroidism is a pathological decline in thyroid function characterized by elevated TSH and metabolic slowing, often felt as a deep chill. Because estrogen influences thyroid binding proteins, distinguishing between Menopause vs. Hypothyroidism requires a comprehensive panel testing TSH, Free T4, Free T3, TPO Antibodies, FSH, and Estradiol.
The Midlife Medical Gray Area
Why is this diagnosis so difficult to pin down? The challenge lies in the subtlety of the symptoms during the early stages. When a woman enters perimenopause, her estrogen does not just drop. It fluctuates wildly.
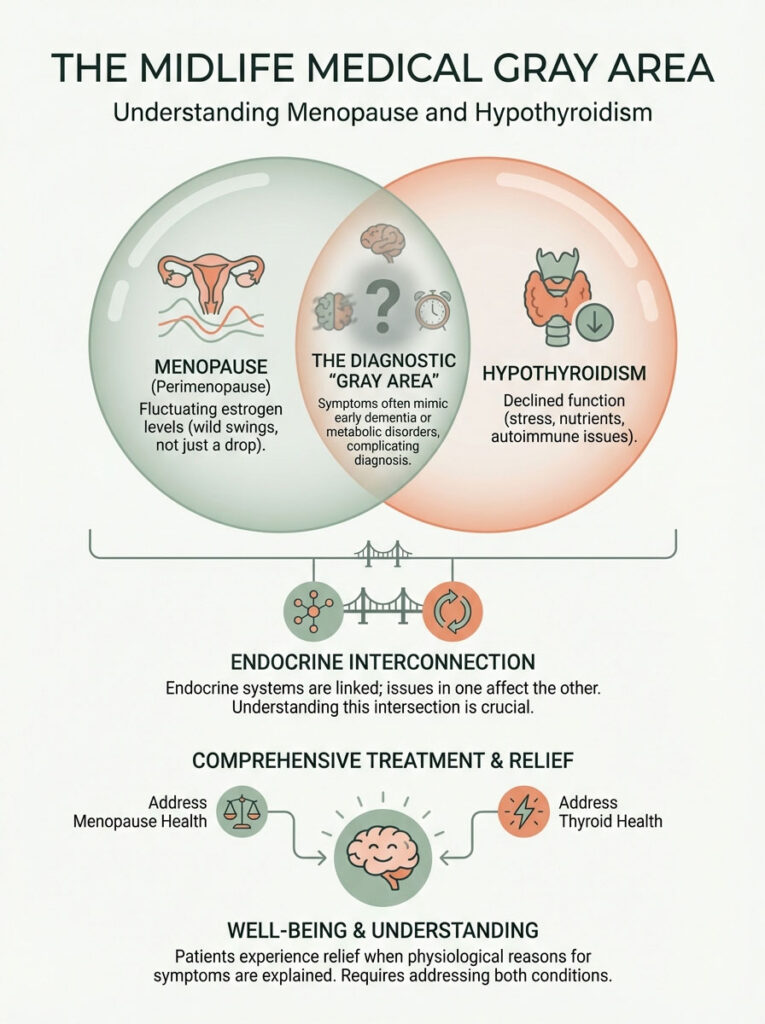
These fluctuations create a chaotic signaling environment in the body. Simultaneously, the thyroid gland often begins to struggle. This is due to decades of stress, nutrient depletion, or autoimmune activation. Patients often come to me convinced they have early dementia or a metabolic disorder.
They are relieved to learn that there is a physiological reason for their suffering. The intersection of Menopause vs. Hypothyroidism is not just bad luck. It is a biological collision. The ovaries and the thyroid are part of the endocrine system’s delicate web. When one strand vibrates, the whole web shakes.
Standard medical training often treats these systems in silos. An endocrinologist looks at the thyroid. A gynecologist looks at the ovaries. In my practice, we look at the crosstalk between the two. If we treat the menopause but ignore the thyroid, you will still feel tired. If we treat the thyroid but ignore the estrogen loss, you will still have brain fog. We must address both.
The Biological Intersection: Why Now?
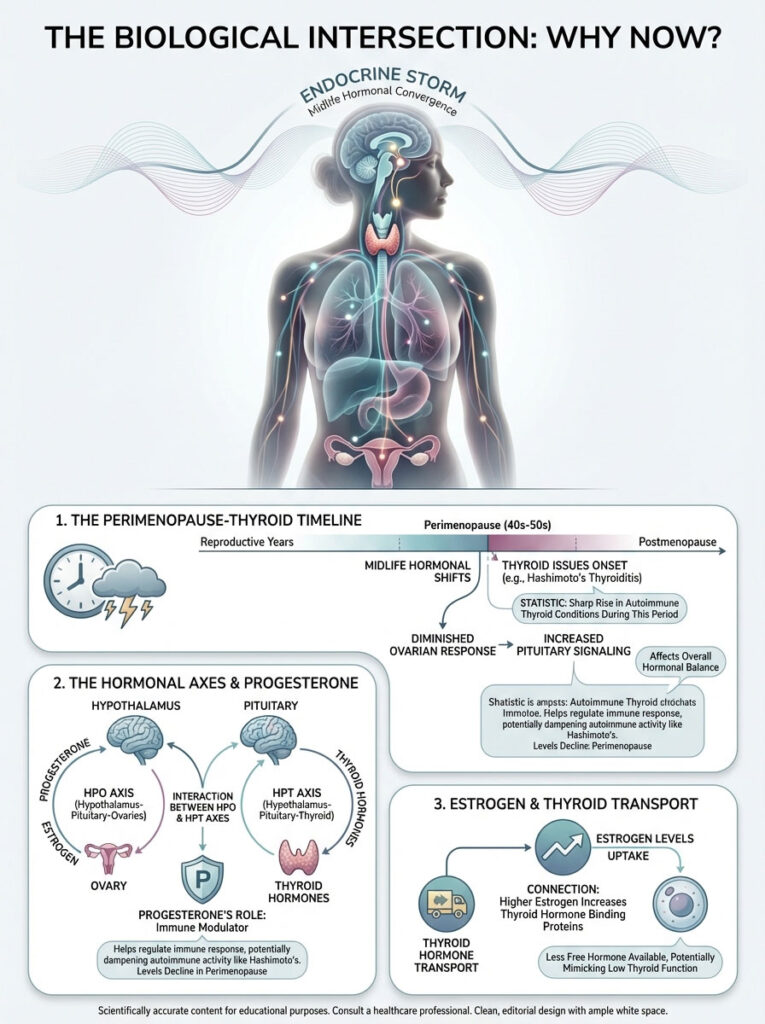
To understand why you feel this way, we have to look at the “Endocrine Storm” that occurs in the fourth and fifth decades of life. It is rarely a coincidence that thyroid issues surface just as periods become irregular.
Key Statistics: The Midlife Convergence
- 1 in 8: The number of women who will develop a thyroid disorder in their lifetime (American Thyroid Association).
- Peak Onset: Hashimoto’s Thyroiditis diagnosis peaks between ages 40 and 60, perfectly overlapping with perimenopause.
- 60%: The percentage of people with thyroid disease who are unaware of their condition.
- Symptoms Overlap: Approximately 70% of hypothyroid symptoms mimic perimenopausal symptoms.
- 4 Years: The average time it takes for a woman to receive a correct diagnosis for autoimmune conditions.
- 5x to 8x: Women are five to eight times more likely than men to have thyroid problems.
The Age Factor and Immune Sensitivity
The onset of perimenopause usually begins in the early to mid-40s. This is a time when ovarian reserve diminishes. Coincidentally, this is the exact age range where autoimmune thyroid disease tends to manifest.
Specifically, we see a rise in Hashimoto’s Thyroiditis. The immune system is highly sensitive to hormonal changes. Progesterone is a natural immune modulator. It calms the immune system down. As progesterone drops in perimenopause, the immune system may become more aggressive. This can lead to an attack on the thyroid gland.
Mechanisms of Action: The HPO and HPT Axes
The body relies on two primary axes for energy and regulation. First is the Thyroid Axis (HPT). The thyroid is the master control of your Basal Metabolic Rate (BMR). It dictates how fast your cells burn energy.
Second is the Ovarian Axis (HPO). This regulates reproduction and thermoregulation (body temperature control). These systems do not operate independently. They communicate via the pituitary gland in the brain. The pituitary sends TSH to the thyroid. It sends FSH to the ovaries.
When the ovaries stop responding to the signal, the pituitary screams louder. This results in high FSH. This stress on the pituitary can confuse the signaling to the thyroid. Furthermore, estrogen directly impacts how thyroid hormones are transported in the blood. When we look at Menopause vs. Hypothyroidism, we are looking at a failure of communication in the control tower of the brain.
Symptom Decoding: The Thermoregulation Cluster
If you search online, you will find lists of symptoms that look identical. Fatigue. Weight gain. Hair loss. To really distinguish between the two, we have to analyze the quality of the symptom. How does it feel in your body?

Vasomotor Instability vs. Metabolic Slowing
Temperature regulation is the most telling sign. In perimenopause, the hallmark is the “hot flash.” This is a sudden, intense wave of heat caused by estrogen withdrawal. It destabilizes the hypothalamus. It feels like internal combustion. You want to rip your clothes off. It passes in minutes.
In contrast, hypothyroidism causes a metabolic slowing. This results in cold intolerance. This is not just feeling chilly. It is a deep, bone-level cold that is hard to shake even under blankets. Patients with low thyroid function often have cold hands and feet. They wear sweaters when others are comfortable. If you are flashing hot one minute and freezing the next, you likely have both issues at play.
Sweating Patterns
The sweat of menopause is often described as “drenching.” It happens particularly at night. It starts from the chest and radiates up. Thyroid skin changes are the opposite.
Hypothyroidism typically leads to dry, cool skin. There is a lack of sweating, even during exertion. If your skin feels like parchment paper and you never sweat, check your thyroid. This dryness extends to the heels, which may crack, and the elbows.
Heart Rate Variability
Perimenopause is often associated with heart palpitations. This is due to adrenaline surges that occur when estrogen drops. Women report their heart “skipping a beat” or racing while resting. It can feel like a panic attack without the panic.
Hypothyroidism generally causes Bradycardia. This is a slow heart rate. If your resting heart rate has dropped below 60 and you feel sluggish, this points toward the thyroid. Your heart simply does not have the energy to pump vigorously.
| Symptom Domain | Perimenopause/Menopause Presentation | Hypothyroidism Presentation |
|---|---|---|
| Thermoregulation | Hot flashes, night sweats, heat intolerance. | Cold intolerance, shivering, cold hands/feet. |
| Weight Pattern | Redistribution to abdomen (visceral fat), loss of muscle tone. | Generalized fluid retention (myxedema), “puffy” appearance. |
| Hair & Skin | Thinning hair (androgenic alopecia), dry vagina, loss of collagen. | Brittle hair, loss of outer eyebrow third, cool/dry/pale skin. |
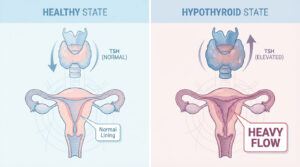
| Menstrual Cycle | Irregular intervals, skipping months, flow varies (light to heavy). | Heavy, prolonged bleeding (Menorrhagia), more frequent cycles. |
| Mood/Cognition | Irritability, rage, “brain fog” due to sleep loss. | Depression, apathy, slowed mental processing speed. |
| Energy Levels | “Tired but wired” (cortisol spikes). | Lethargy, sluggishness, need for excessive sleep. |
The Metabolic Mayhem: Weight Gain Analysis
The number one complaint I hear is weight gain in 40s. It feels unfair. You are eating the same foods you ate at 30. Yet the scale keeps creeping up. This is where distinguishing Menopause vs. Hypothyroidism becomes essential for effective management.
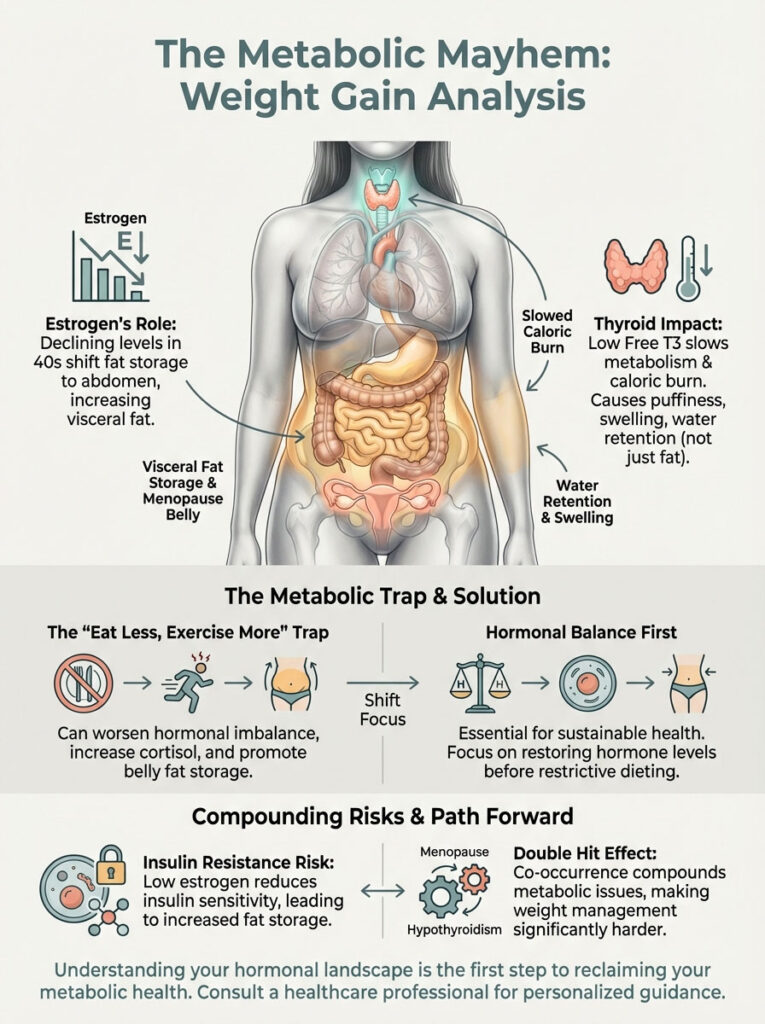
Estrogen and Visceral Fat Storage
Estrogen is a powerful metabolic regulator. When estrogen levels decline, the body panics. Adipose tissue (fat) is capable of producing a weak form of estrogen called estrone. To compensate for the loss of ovarian estrogen, the body attempts to generate more fat cells to produce estrone.
Crucially, this fat storage shifts location. It moves from the subcutaneous layer (hips and thighs) to the visceral area (deep belly fat). This is why many women notice a “menopause belly” or thickening of the waist. This fat is inflammatory and metabolically active. It is not just cosmetic; it is a health risk.
Thyroid and Caloric Burn
Thyroid hormones, specifically Free T3, control the mitochondria. These are the power plants of your cells. When you have hypothyroidism, your mitochondria essentially go on strike. They burn fuel at a much slower rate.
The weight gain associated with low thyroid is often a mix of fat accumulation and water retention. This is known as myxedema. Patients often report feeling “puffy” or swollen all over. It is distinct from just carrying weight in the belly. You might notice your rings don’t fit or your face looks fuller.
Expert Insight: The “Eat Less, Exercise More” Trap
If you are battling Menopause vs. Hypothyroidism, the standard advice to cut calories and do cardio will often backfire. Caloric restriction can further suppress thyroid function (lowering T3). Excessive cardio raises cortisol, which increases belly fat. The solution requires hormonal balancing first, followed by strength training to rebuild the metabolic engine.
The Synergistic Effect of the Double Hit
When a patient has both conditions, it is a “double hit” to the metabolism. The thyroid slows the burn rate. The low estrogen dictates that any stored energy goes straight to the abdomen. This also increases the risk of insulin resistance.
Estrogen helps cells remain sensitive to insulin. Without it, blood sugar rises. This leads to more fat storage. Treating only one side of this equation will result in frustration. You cannot diet your way out of a hormonal problem.
The Autoimmune Link: Hashimoto’s and Hormones
We cannot discuss this topic without addressing Hashimoto’s and menopause. Hashimoto’s Thyroiditis is an autoimmune condition. The body creates antibodies that attack the thyroid gland. It is the leading cause of hypothyroidism in the United States.
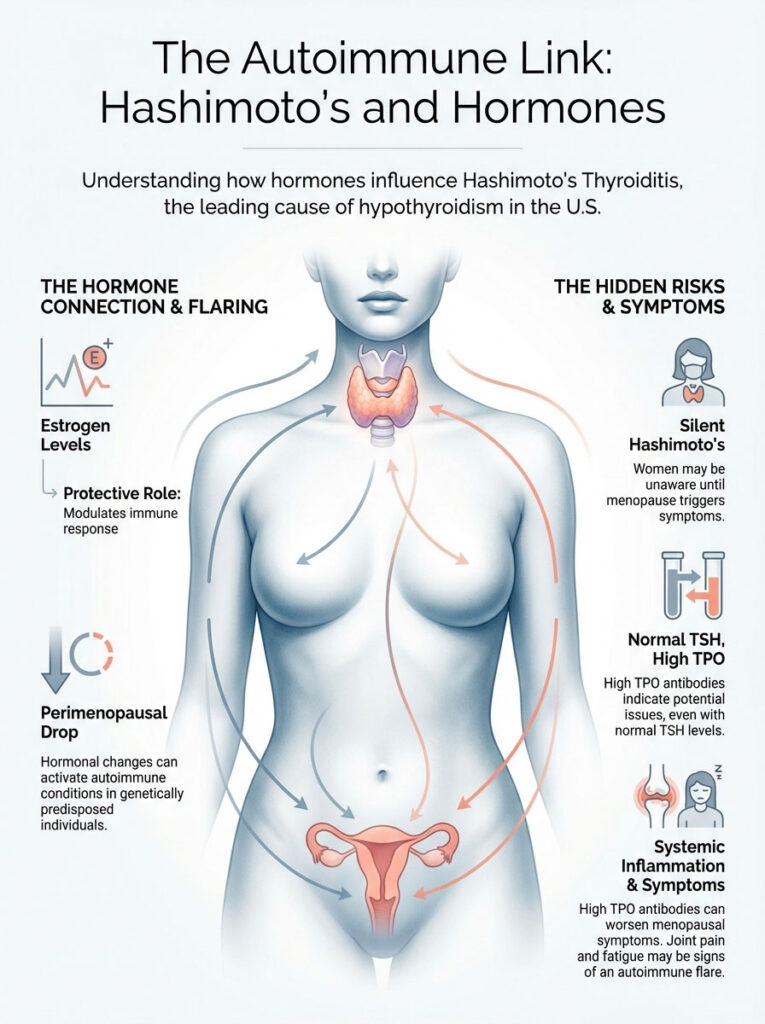
The Protective Role of Estrogen
Why does this condition often flare up during perimenopause? Estrogen has a protective role in the immune system. It helps modulate the immune response. It keeps it from becoming overactive. When estrogen levels become erratic and eventually drop, that “brake pedal” on the immune system is released.
If you have a genetic predisposition to autoimmunity, this hormonal shift can be the trigger. It activates the disease. Many women go their whole lives with silent Hashimoto’s. Then, in their 40s, the drop in hormones wakes the sleeping giant.
TPO Antibodies and Inflammation
Here is a critical clinical detail. A woman can have a “normal” TSH but very high Thyroid Peroxidase (TPO) antibodies. This state produces symptoms like fatigue and joint pain. This happens even before the thyroid gland fully fails.
Standard menopause care often misses this. If you are experiencing joint pain (often blamed on menopause), it is vital to check for TPO antibodies. You must rule out an autoimmune flare. High antibodies indicate systemic inflammation. This inflammation can make menopausal symptoms like brain fog significantly worse.
Diagnostic Biomarkers: The “Dr. Vance” Panel
If you suspect you are dealing with Menopause vs. Hypothyroidism, you need data. Subjective feelings are important. However, blood work provides the roadmap. The biggest mistake I see is doctors ordering only a TSH test.
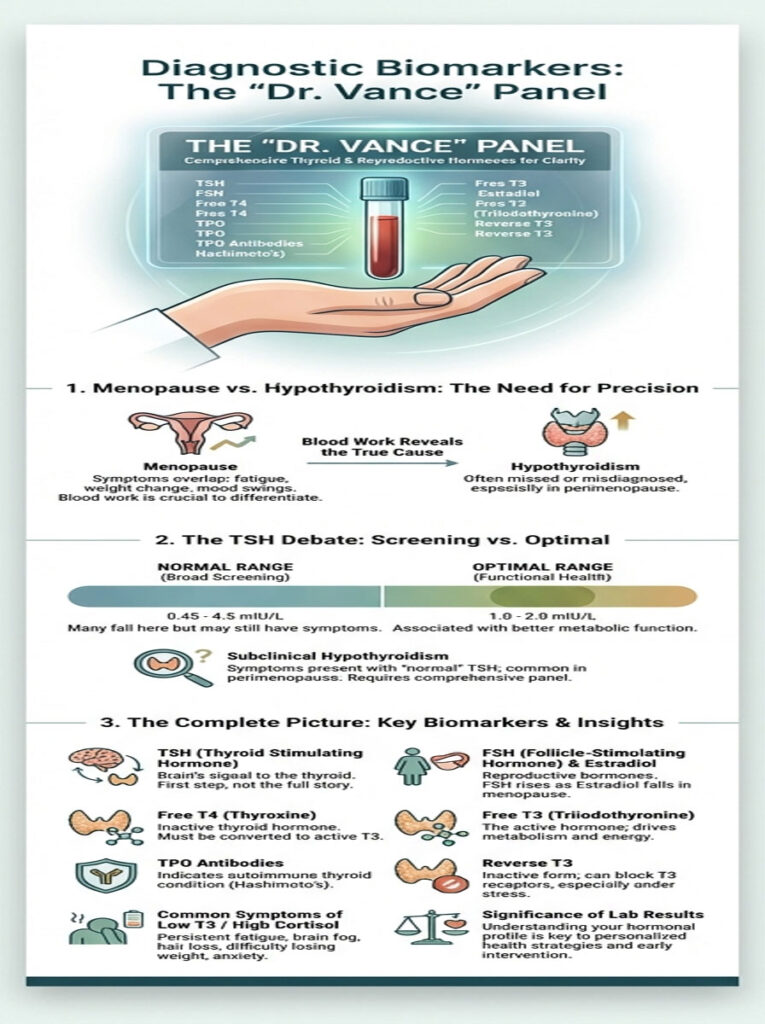
The Fallacy of TSH Screening
TSH (Thyroid Stimulating Hormone) is a pituitary hormone. It is not a thyroid hormone. It tells us how loud the brain is yelling at the thyroid. While it is a good screening tool, it is insufficient for symptomatic midlife women.
You can have a normal TSH but have low levels of active thyroid hormone (T3) available to your cells. This is common in women with high cortisol or liver congestion. The brain thinks everything is fine, but the cells are starving for energy.
Defining “Optimal” vs. “Normal”
Lab ranges are based on a bell curve of the population. The “normal” range for TSH is typically 0.45 to 4.5 mIU/L. However, most women feel best when their TSH is between 1.0 and 2.0. If your TSH is 4.2, you are technically “normal.” But you likely feel terrible.
We call this “subclinical hypothyroidism.” In perimenopause, it is worth treating. To truly understand your status, you must request a full thyroid panel alongside your reproductive hormones.
| Biomarker | What It Measures | Menopause Pattern | Hypothyroidism Pattern |
|---|---|---|---|
| TSH | Pituitary signal to thyroid. | Normal (usually). | Elevated (> 4.5 mIU/L). |
| FSH | Pituitary signal to ovaries. | Elevated (> 30 mIU/mL). | Normal. |
| Estradiol | Main estrogen hormone. | Low/Fluctuating. | Normal (unless severe). |
| Free T4 | Storage thyroid hormone. | Normal. | Low. |
| Free T3 | Active thyroid hormone. | Normal. | Low (Metabolic slowing). |
| TPO Antibodies | Immune attack on thyroid. | Negative. | Positive (Hashimoto’s). |
| Reverse T3 | “Brake pedal” hormone. | Normal. | Elevated (stress/inflammation). |
The Critical Interaction: HRT and Thyroid Medication
This section is perhaps the most important for anyone already taking medication. There is a direct, biochemical interaction between Hormone Replacement Therapy (HRT) and thyroid medication like Levothyroxine. Understanding this can prevent months of misery.
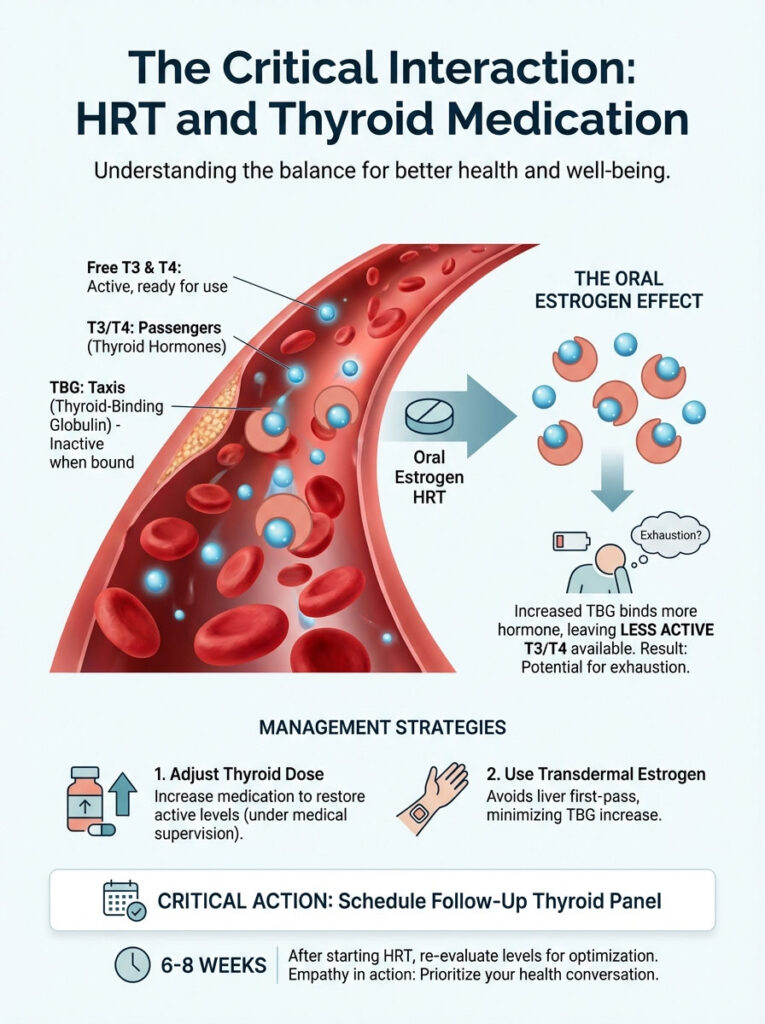
Thyroid Binding Globulin (TBG): The Taxi Analogy
To understand this, think of thyroid hormones as passengers. Think of the proteins in your blood as taxis. These taxis are called Thyroid Binding Globulin (TBG). When thyroid hormone is inside the taxi (bound), it is inactive. It cannot enter your cells to give you energy. It is just riding around in the bloodstream.
Only when it steps out of the taxi (free) does it work. This is why we measure “Free T3” and “Free T4.” We want to know how many passengers are walking on the sidewalk, ready to work. Not how many are stuck in traffic.
When you take oral estrogen (pills), it is processed by the liver. This “first pass” through the liver stimulates the production of more TBG. Suddenly, you have a fleet of empty taxis. They pick up all your free thyroid hormone. Even if you are taking your Levothyroxine faithfully, the oral estrogen binds it up. It makes it unavailable to your body.
Clinical Consequence and Management
I frequently see women who have been stable on thyroid medication for years. They start oral HRT for hot flashes. Four weeks later, they feel exhausted and hypothyroid again. Their doctor might think the HRT isn’t working. In reality, the HRT has effectively lowered their thyroid dose.
There are two ways to manage this interaction. First, we can adjust the thyroid dose. If a woman must take oral estrogen, we often need to increase her Levothyroxine. This compensates for the increased binding proteins.
Second, and preferably, we change the route of administration. Transdermal estrogen, patches, gels, or sprays, absorbs directly into the bloodstream. It bypasses the liver. This avoids the spike in Thyroid Binding Globulin (TBG). It leaves thyroid levels largely unaffected. If you are starting HRT, always schedule a follow-up full thyroid panel 6 to 8 weeks later.
Hair Loss: The Distinct Patterns
Hair loss is emotional. It is often the symptom that finally drives a woman to the doctor. Both conditions cause it, but they look different.
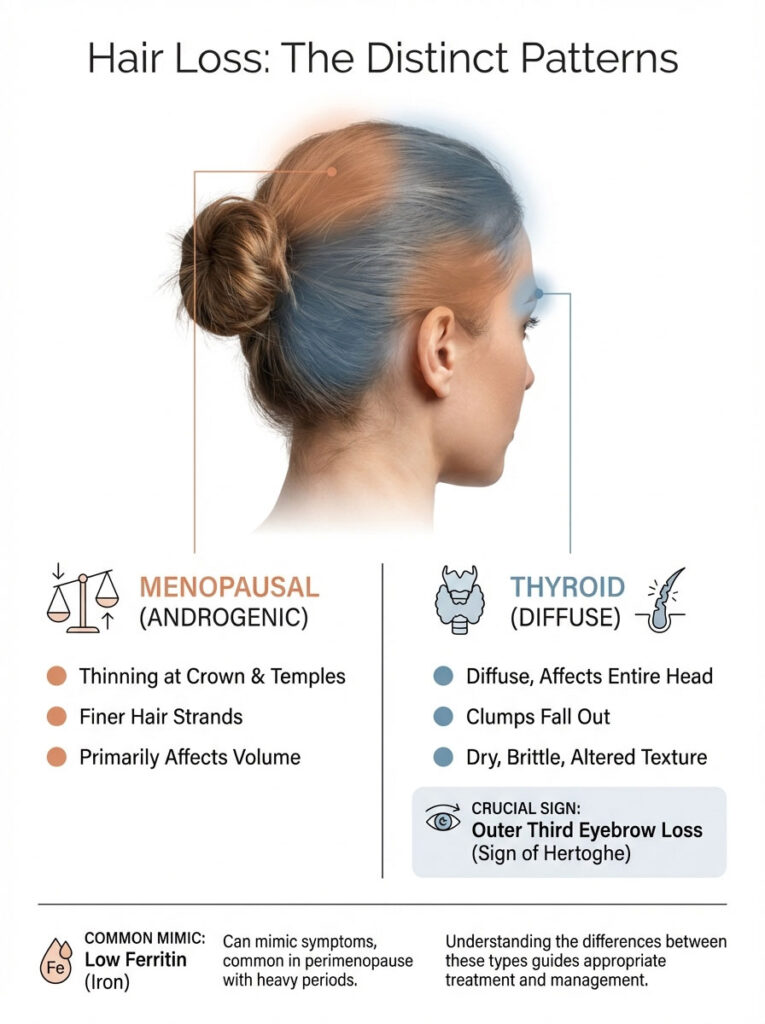
The Menopausal Shed
Menopausal hair loss is typically “androgenic.” As estrogen drops, testosterone becomes relatively more dominant. This can shrink hair follicles. You will notice thinning specifically at the crown of the head and the temples. The part in your hair might look wider. The individual strands may become finer.
The Thyroid Shed
Thyroid hair loss is often diffuse. It happens all over the head. You might find clumps of hair in the shower drain. It is not limited to the top of the head. Crucially, look at your eyebrows. Hypothyroidism often causes the loss of the outer third of the eyebrows. This is a classic clinical sign called the “Sign of Hertoghe.”
Furthermore, thyroid hair tends to be dry, brittle, and straw-like. Menopausal hair loss is usually about volume. Thyroid hair loss is about texture and volume. I also recommend checking Ferritin (iron storage). Low iron mimics both of these conditions and is common in perimenopausal women with heavy periods.
Brain Fog: Memory vs. Processing
Cognitive decline is a terrifying prospect. Many women fear early-onset Alzheimer’s. Distinguishing the source of the “fog” can be reassuring.
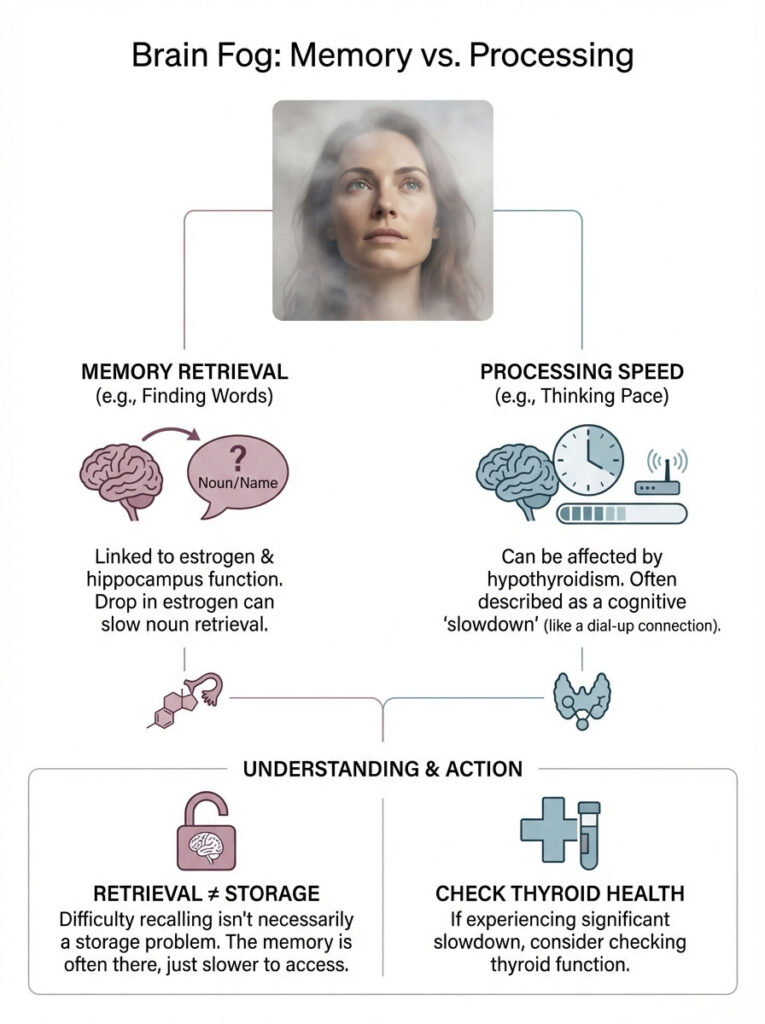
Estrogen and Verbal Recall
Estrogen is vital for the hippocampus. This is the memory center of the brain. When estrogen drops, women often struggle with “noun retrieval.” You know the word for “stapler,” but you can’t find it. You might forget names of people you know well. This is frustrating, but it is usually a retrieval issue, not a storage issue.
Thyroid and Processing Speed
Hypothyroidism affects the speed of neural transmission. Patients describe it as feeling “drugged” or moving through molasses. It is not just forgetting a word; it is a difficulty in focusing on a task or following a complex conversation. It is a slowing of mental processing. If you feel like your brain is operating on a dial-up connection instead of fiber optic, check your thyroid.
Treatment Protocols: An Integrative Approach
Treating Menopause vs. Hypothyroidism is not an “either/or” situation. It is usually “both/and.” We need an integrative protocol that supports both axes.
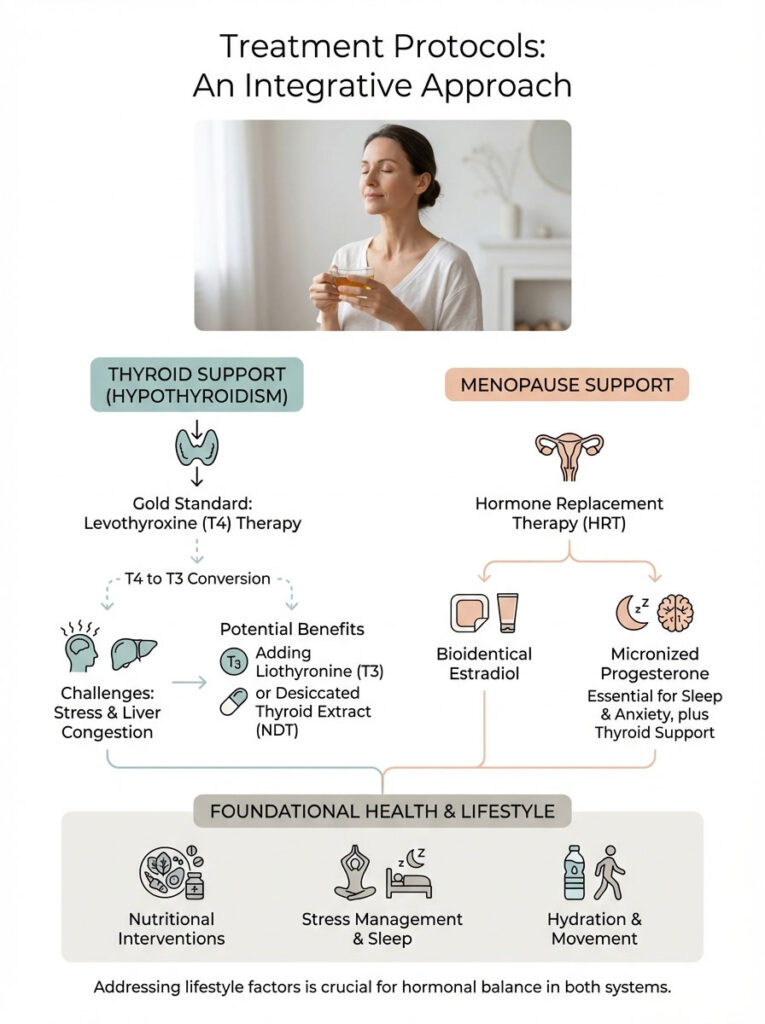
Standard of Care (Thyroid)
The gold standard for hypothyroidism is Levothyroxine (synthetic T4). However, many perimenopausal women have trouble converting T4 into the active T3 hormone. This is due to stress and liver congestion.
In these cases, T4 monotherapy may leave you feeling symptomatic. Adding a small amount of Liothyronine (synthetic T3) can make a profound difference. Some patients also do well on desiccated thyroid extract (NDT), which contains both T4 and T3 naturally.
Standard of Care (Menopause)
Hormone Replacement Therapy (HRT) is the most effective treatment for vasomotor symptoms. We typically use bioidentical Estradiol. Transdermal is preferred for the reasons mentioned above.
We also use micronized Progesterone. Progesterone is essential not just for protecting the uterus. It is also vital for sleep and anxiety reduction. Interestingly, progesterone can also support thyroid signaling. It increases TPO activity, making it a win-win for the thyroid patient.
Nutritional Interventions
Pills alone rarely fix everything. We must build a foundation of health through nutrition.
- Selenium and Zinc: These minerals are critical for the conversion of T4 to T3. Brazil nuts are a potent source of selenium. Just two a day can provide your daily need. Zinc is found in pumpkin seeds and oysters.
- Gluten and Autoimmunity: For women with Hashimoto’s, gluten can be a trigger. The molecular structure of gliadin (gluten protein) resembles thyroid tissue. This is called molecular mimicry. Eating gluten can confuse the body into attacking the thyroid. A trial of being gluten-free is often recommended.
- Phytoestrogens: Foods like flaxseeds and fermented soy can act as weak estrogens. They can help modulate menopausal symptoms. However, separate soy intake from thyroid medication by at least 4 hours.
- Gut Health: 20% of your thyroid hormone conversion happens in the gut. Probiotics and fermented foods support this process. A healthy gut also helps clear excess estrogen, preventing dominance.
Lifestyle Interventions (Dual Benefit)
We must address the lifestyle factors that sabotage both systems.
- Stress Management: Cortisol is a bully. It steals resources from the thyroid pathway. It also exacerbates hot flashes. Breathwork, meditation, or simply saying “no” to excessive obligations is medical therapy in this stage of life.
- Exercise: Muscle is the organ of longevity. Strength training counteracts the muscle loss (sarcopenia) caused by both low estrogen and low thyroid. It also improves insulin sensitivity. This combats the weight gain in 40s. Prioritize lifting heavy things over long-distance running.
- Sleep Hygiene: Both conditions disrupt sleep. Keep the room cool (65 degrees). Use blackout curtains. Magnesium glycinate before bed can help with both relaxation and hormone metabolism.
Case Studies: Clinical Applications
To illustrate how this looks in the real world, let’s review three cases from my practice (names changed for privacy).
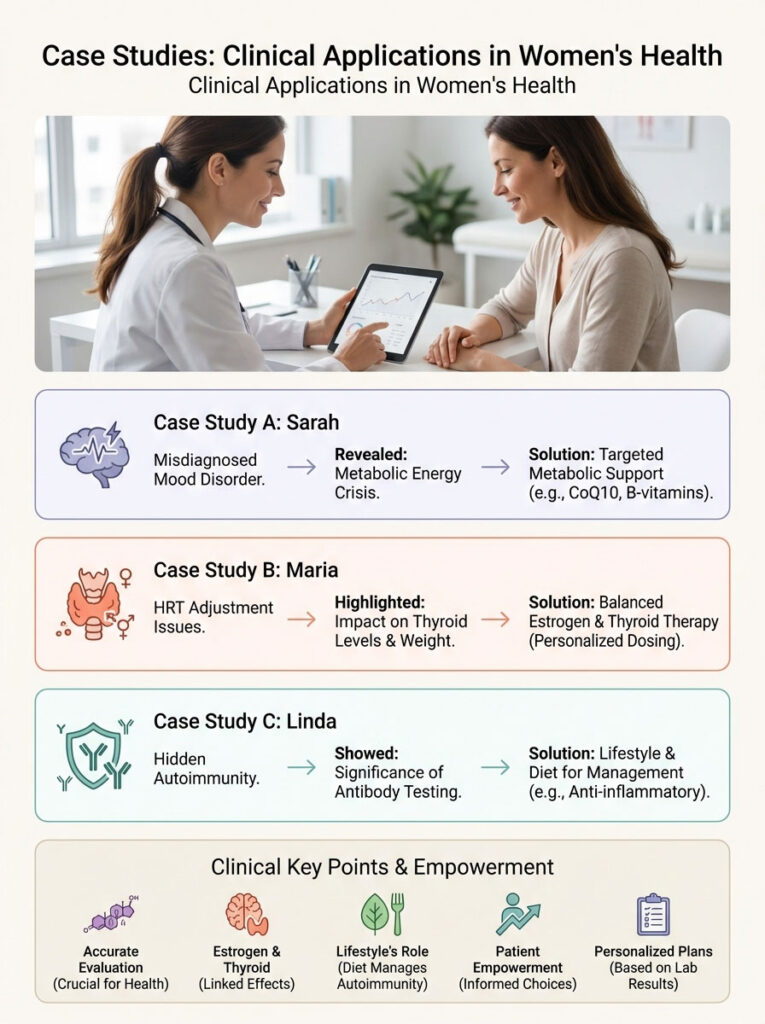
Case Study A: “The Misdiagnosed Mood Disorder”
Sarah, 48, came to me on antidepressants. She had been diagnosed with “midlife depression.” She was sleeping 10 hours a night but waking up unrefreshed. She was gaining weight and feeling apathetic. Her periods were irregular.
Her TSH was 3.8. This is technically normal in many labs. However, her Free T3 was at the very bottom of the range. Her Estradiol was low. She didn’t have clinical depression; she had a metabolic energy crisis. We started her on a low dose of thyroid support and transdermal estrogen. Within three months, the “depression” lifted. She had the energy to return to the gym.
Case Study B: “The HRT Adjustment”
Maria, 52, had known Hashimoto’s for years. She was well-managed on Levothyroxine. When menopause hit, her primary doctor put her on an oral estrogen pill. Within a month, her hair started falling out. She gained 8 pounds.
She thought the HRT was causing weight gain. We ran her labs. Her TSH had spiked to 7.0 because the oral estrogen increased her Thyroid Binding Globulin (TBG). We switched her to an estrogen patch. Her thyroid levels normalized without changing her thyroid dose. The weight stabilized.
Case Study C: “The Hidden Autoimmunity”
Linda, 45, complained of joint pain and “feeling old.” Her periods were fine. Her TSH was perfect at 1.5. Her doctor told her it was just aging. We ran a full panel including antibodies.
Her TPO antibodies were over 600. She was in the early stages of Hashimoto’s, triggered by perimenopausal stress. Her thyroid was still pumping out hormone, but her body was inflamed. We put her on a gluten-free diet and Low Dose Naltrexone (LDN) to modulate her immune system. The joint pain vanished in weeks.
Summary & Key Takeaways
The journey through midlife does not have to be a miserable descent into fatigue and brain fog. While the overlap between Menopause vs. Hypothyroidism is complex, it is logical and treatable. The symptoms overlap because the biological systems are connected.
The heat of menopause and the cold of hypothyroidism can exist in the same body. This creates a confusing picture that requires expert interpretation. You do not have to choose which one to treat. You often need to treat both.
Actionable Steps for You:
- Track Your Symptoms: Note your temperature tolerance. Are you flashing heat or freezing cold? Check your eyebrows and your resting heart rate.
- Demand the Data: Do not accept a TSH-only screening. Request a full thyroid panel including Free T3, Free T4, Reverse T3, and TPO antibodies.
- Check the Interaction: If you are on thyroid meds and starting HRT, ask for transdermal estrogen. This protects your thyroid availability.
- Monitor Regularly: These are dynamic conditions. What worked last year might need adjustment this year. Test every 6 months during the transition.
- Prioritize Muscle: Shift your exercise focus from cardio to strength training. This protects your metabolism against the decline of both hormones.
You know your body better than anyone else. If you are told you are “normal” but you do not feel that way, keep asking questions. It is not just “getting older” it is likely a treatable hormonal imbalance. You deserve to feel vibrant in your 40s, 50s, and beyond.
Frequently Asked Questions
How can I tell the difference between menopause hot flashes and thyroid-related temperature changes?
Menopause hot flashes are sudden, intense waves of internal heat caused by estrogen withdrawal that typically pass within minutes. In contrast, hypothyroidism causes a deep, bone-level cold intolerance and cold extremities due to a slowed basal metabolic rate. If you are experiencing drenching night sweats followed by a persistent chill that requires extra blankets, you likely have both conditions occurring simultaneously.
Why is my TSH normal if I still have all the symptoms of hypothyroidism and menopause?
Standard laboratory “normal” ranges for TSH are often too broad, covering a wide bell curve of the population rather than an optimal health state. Many women in perimenopause feel their best when TSH is between 1.0 and 2.0 mIU/L, yet they are told they are fine even at a 4.2. Furthermore, a TSH test alone misses issues with T4 to T3 conversion, which is common during the hormonal shifts of midlife.
Can starting hormone replacement therapy affect my thyroid medication dose?
Yes, oral estrogen therapy increases the production of Thyroid Binding Globulin (TBG) in the liver, which acts like a sponge that soaks up your active thyroid hormone. If you are taking Levothyroxine, starting an oral estrogen pill may require an increase in your thyroid dose to maintain the same level of metabolic function. Using transdermal estrogen patches or gels is often preferred because they bypass the liver and do not interfere with thyroid binding.
What specific blood tests should I request to distinguish between menopause and hypothyroidism?
To get a clear clinical picture, you must move beyond a simple TSH screening and request a full panel including Free T4, Free T3, Reverse T3, and TPO Antibodies. To assess ovarian function at the same time, we also test FSH and Estradiol levels. This comprehensive data allows us to identify if your symptoms are driven by ovarian decline, thyroid failure, or an autoimmune flare-up like Hashimoto’s.
Does menopause trigger autoimmune conditions like Hashimoto’s thyroiditis?
Perimenopause is a high-risk window for the onset of Hashimoto’s because progesterone, which acts as a natural immune modulator, begins to decline. When this “brake pedal” on the immune system is removed, genetically predisposed women may experience an autoimmune attack on the thyroid gland. It is common for “silent” thyroid issues to become symptomatic during the exact years that menstrual cycles become irregular.
Why am I gaining weight specifically in my midsection during perimenopause?
Weight gain in the 40s is often a “double hit” from both endocrine systems; low estrogen causes the body to store visceral fat in the abdomen to produce estrone, while low thyroid hormone slows down mitochondrial calorie burning. This shift is not just about calories, but about insulin resistance and metabolic slowing. Addressing both the estrogen deficit and the thyroid sluggishness is required to successfully shift this stubborn belly fat.
Is my hair loss caused by dropping estrogen or a thyroid imbalance?
Menopausal hair loss typically presents as “androgenic” thinning at the crown and temples, where the hair part becomes wider over time. Thyroid-related hair loss is usually diffuse across the entire scalp and often includes a unique clinical sign called the Sign of Hertoghe, which is the thinning of the outer third of the eyebrows. If your hair feels brittle and straw-like and is falling out in clumps, the thyroid is the more likely culprit.
How does thyroid-related brain fog differ from menopausal memory lapses?
Menopausal brain fog is often characterized by “noun retrieval” issues, where you know the word you want but cannot find it. Thyroid-related cognitive decline is more about mental processing speed, making you feel as though your brain is moving through molasses or is “drugged.” While estrogen loss affects memory storage in the hippocampus, low thyroid hormone slows down the actual speed of neural transmissions.
What is the best way to take estrogen if I am also on Levothyroxine?
I strongly recommend transdermal estradiol—delivered via a patch, gel, or spray—for women who are also managing hypothyroidism. Because these forms absorb directly through the skin, they do not trigger the liver to produce excess binding proteins that would otherwise deactivate your thyroid medication. This approach allows for stable hormone replacement without the need for constant thyroid dose adjustments.
Why do I feel “tired but wired” during the menopause transition?
The “tired but wired” feeling is a classic symptom of the HPA axis being overtaxed by both thyroid sluggishness and estrogen fluctuations. When your thyroid isn’t providing enough cellular energy, your body compensates by pumping out adrenaline and cortisol to keep you going. This results in a state of exhaustion where you are physically spent but your nervous system is too agitated to allow for deep, restorative sleep.
Can a gluten-free diet help with both menopausal and thyroid symptoms?
For women with Hashimoto’s, gluten can trigger “molecular mimicry,” where the immune system confuses gluten proteins with thyroid tissue, worsening the autoimmune attack. Reducing this systemic inflammation can significantly alleviate joint pain and brain fog that are often incorrectly blamed on menopause. Eliminating gluten helps calm the immune system, allowing your hormonal treatments to work more effectively.
Why is my heart racing or skipping beats during perimenopause?
Heart palpitations are a very common symptom of perimenopause caused by adrenaline surges that happen when estrogen levels drop suddenly. However, hypothyroidism usually causes a slow heart rate, known as bradycardia. If you notice your heart racing while at rest, it is likely an estrogen-related vasomotor symptom, but if your resting heart rate has dropped significantly, we need to check your thyroid function.
Disclaimer
This article is for informational purposes only and does not constitute medical advice, diagnosis, or treatment. The interaction between reproductive hormones and thyroid function is complex and varies by individual. Always consult with a qualified healthcare professional or a certified menopause practitioner before starting Hormone Replacement Therapy (HRT) or changing thyroid medication dosages.
References
- American Thyroid Association – thyroid.org – Provides clinical guidelines on the prevalence of thyroid disorders in women and diagnostic standards for hypothyroidism.
- The North American Menopause Society (NAMS) – menopause.org – Authoritative source for perimenopause symptoms, HRT safety, and the “certified menopause practitioner” standards.
- Endocrine Society – endocrine.org – Detailed research on the HPO and HPT axes and how estrogen influences thyroid-binding globulin (TBG) in the liver.
- Journal of Clinical Endocrinology & Metabolism – “The Impact of Exogenous Estrogens on Thyroid Function” – Peer-reviewed study detailing the interaction between oral HRT and Levothyroxine absorption.
- Hashimoto’s Thyroiditis: A Review – PubMed/National Institutes of Health – Clinical data on the peak onset of autoimmune thyroiditis in women aged 40-60.
- Mayo Clinic – mayoclinic.org – Comparative analysis of vasomotor symptoms versus metabolic slowing in midlife women.