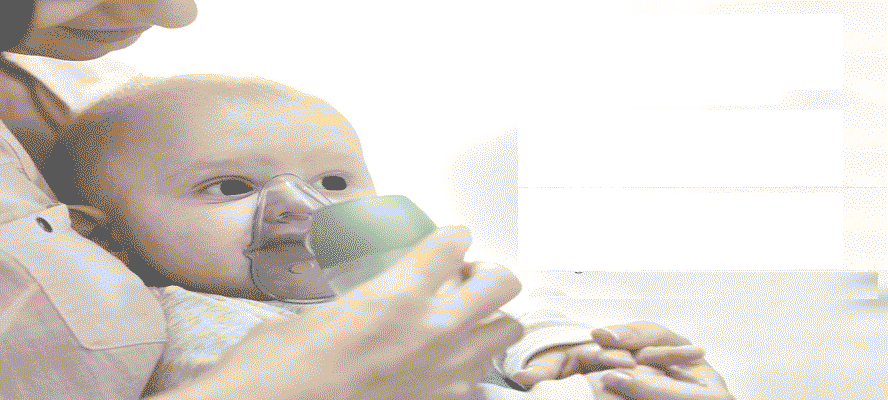
Today, Due to environmental conditions, pre-pregnancy pulmonary infections, lifestyle habits like Smoking, junk food, the ability to withstand the intra-uterine and extrauterine turbulence is critically altered in the past couple of decades. Accordingly, studies have revealed that almost 35% of neonates face breathing difficulties, and need assisted ventilation. even above 28 weeks of gestation. Surprisingly, the data excludes neonates who are born with congenital abnormalities and other common conditions seen in infants. Enough evidences gathered through several studies are also supporting the fact that there has been an exponential increase in several neonatal admission postpartum; due to increased respiratory complications in mothers as well as due to increased rate of c-section deliveries. Although, due to increased technological advancements and contemporary diagnostic facilities, the mortality rate has severely decreased over the period prompt administration of effective treatment regimens is highly crucial for better clinical outcomes.