You track every calorie. You hit the gym four times a week. You prioritize sleep, yet the scale stays frozen while your energy crashes before noon.
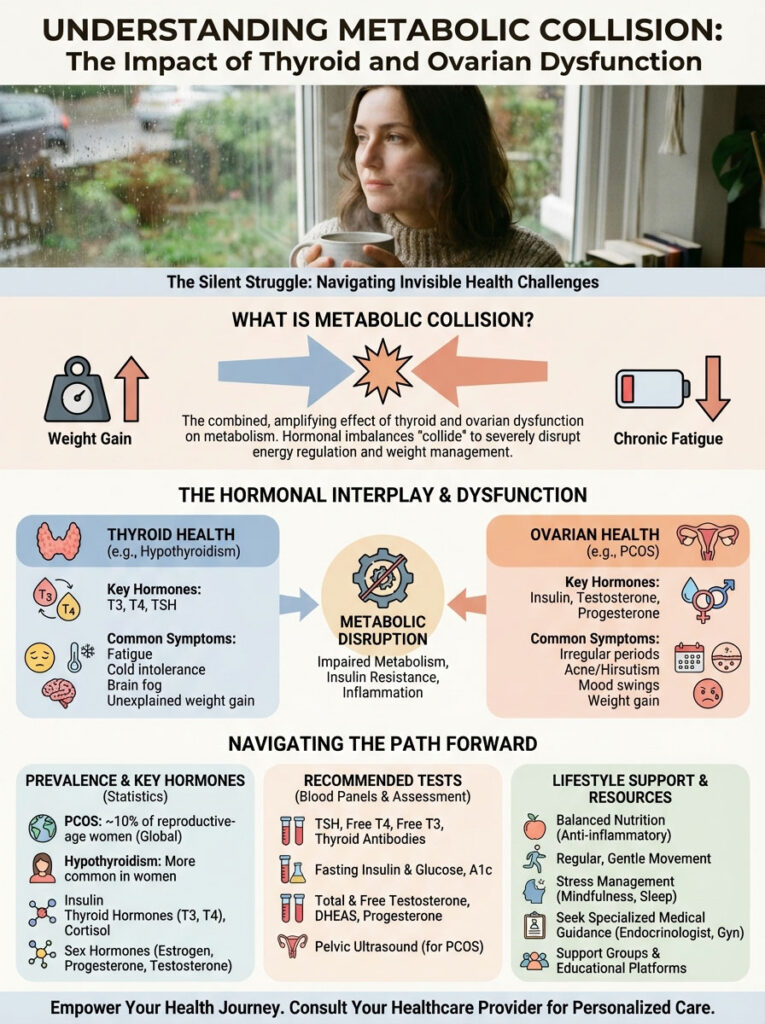
This isn’t a lack of willpower, and you aren’t imagining the struggle. You are likely the victim of a metabolic collision that most general practitioners completely overlook.
When your thyroid and ovaries malfunction simultaneously, they create a “double hit” that locks your metabolism in storage mode. Here is why your body is fighting you and the specific numbers you need to check to win the war.
Want to make better decisions? Read the full article: PCOS and Hypothyroidism: How to Manage the Double Link?
The Hidden “Sponge” Mechanism
Your liver produces a crucial protein called Sex Hormone-Binding Globulin (SHBG). Think of this protein as a safety sponge.
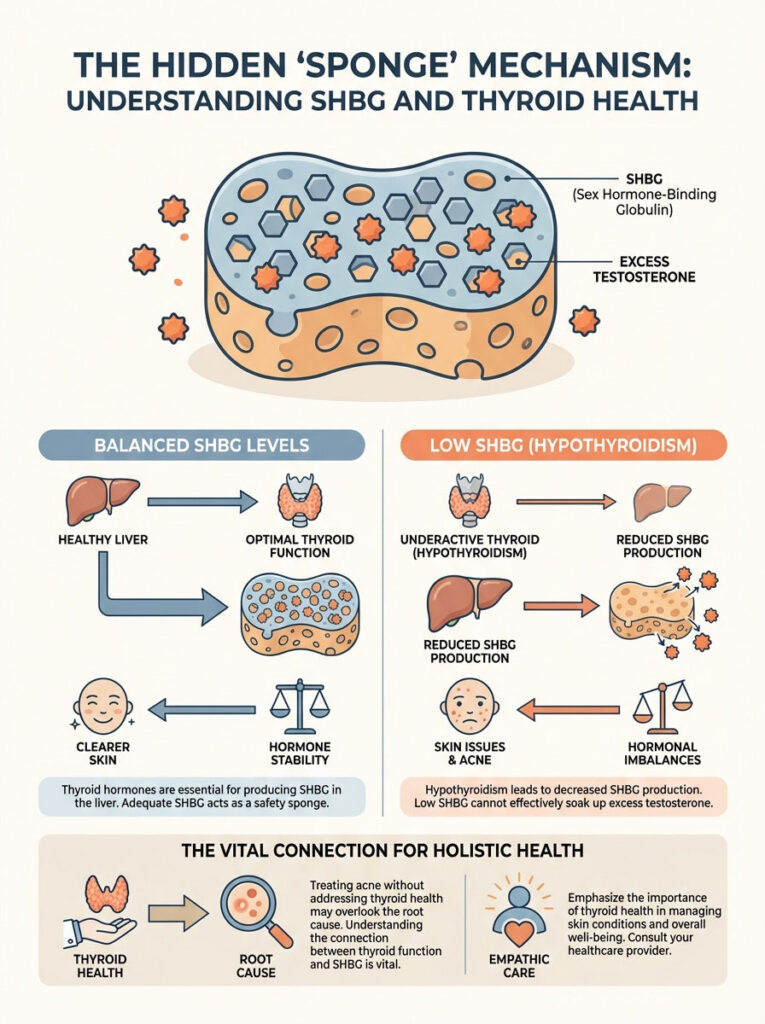
Its job is to soak up excess testosterone in your blood. When the sponge works, your skin stays clear and your hormones remain balanced.
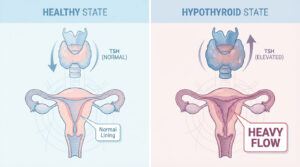
However, thyroid hormones are the factory workers that build these sponges. When your thyroid slows down (hypothyroidism), your liver stops making enough SHBG.
The Consequence of Low SHBG
- Free Testosterone Spikes: Without the sponge, androgen levels surge.
- Adult Acne: Cystic breakouts appear along the jawline.
- Hirsutism: Dark, coarse hair grows where it shouldn’t.
I have seen countless women treat the acne without realizing their sluggish thyroid is the arsonist starting the fire.
Insulin: The Thyroid Bully
Most women with PCOS battle insulin resistance. This means your body screams for more insulin just to process a simple meal.

This excess insulin is toxic to your thyroid gland. It acts as a growth factor, physically enlarging the gland and causing nodules or goiters.
Even worse, high insulin triggers inflammation that can flip the switch on autoimmunity. This is why women with PCOS are three times more likely to develop Hashimoto’s disease.
The “Normal” Lab Trap
This is where my patients usually get angry. They go to the doctor, get a blood test, and receive a voicemail saying everything is “normal.”
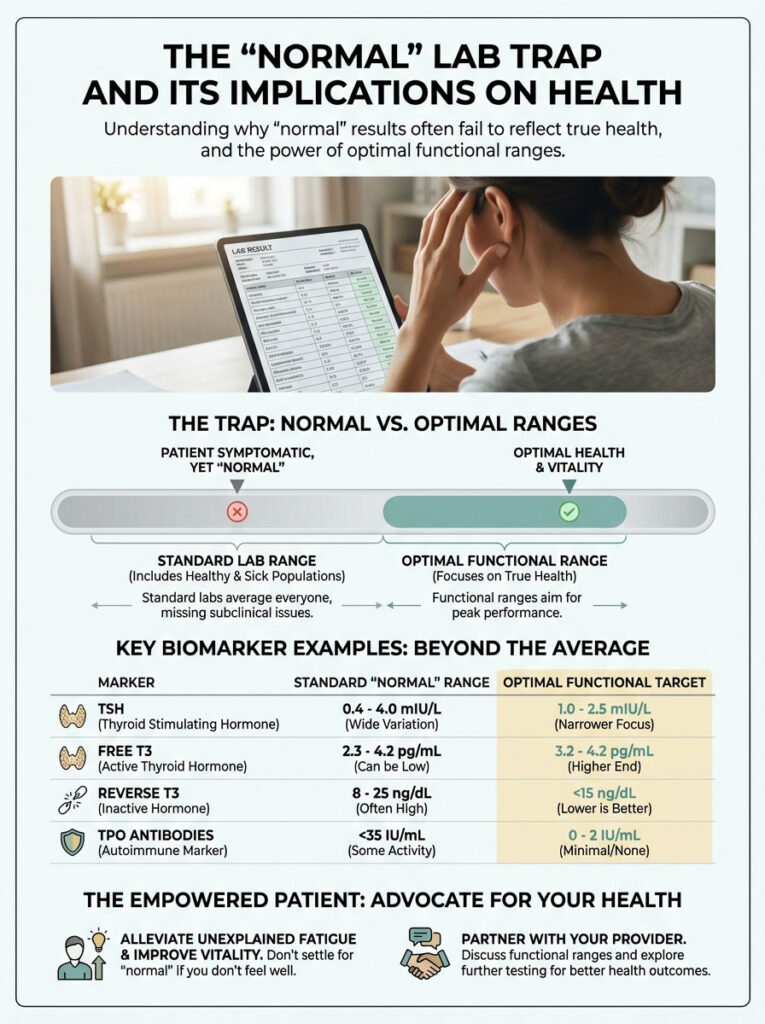
Standard lab ranges are based on the average population, which includes many sick people. Normal is not optimal.
If you want to feel vibrant rather than just “alive,” you must look for functional ranges. I learned this the hard way after years of unexplained fatigue.
The Lab Decoder Ring
| Lab Marker | The “Trap” Range | The Optimal Target |
|---|---|---|
| TSH | 0.4 – 4.5 mIU/L | 0.5 – 2.0 mIU/L |
| Free T3 | Bottom 50% | Upper 25% of range |
| Reverse T3 | Not usually tested | < 15 ng/dL |
| TPO Antibodies | < 35 IU/mL | 0 (Undetectable) |
The Cellular Blockade
Your thyroid makes a storage hormone called T4. It is useless until your body converts it into the active fuel, T3.
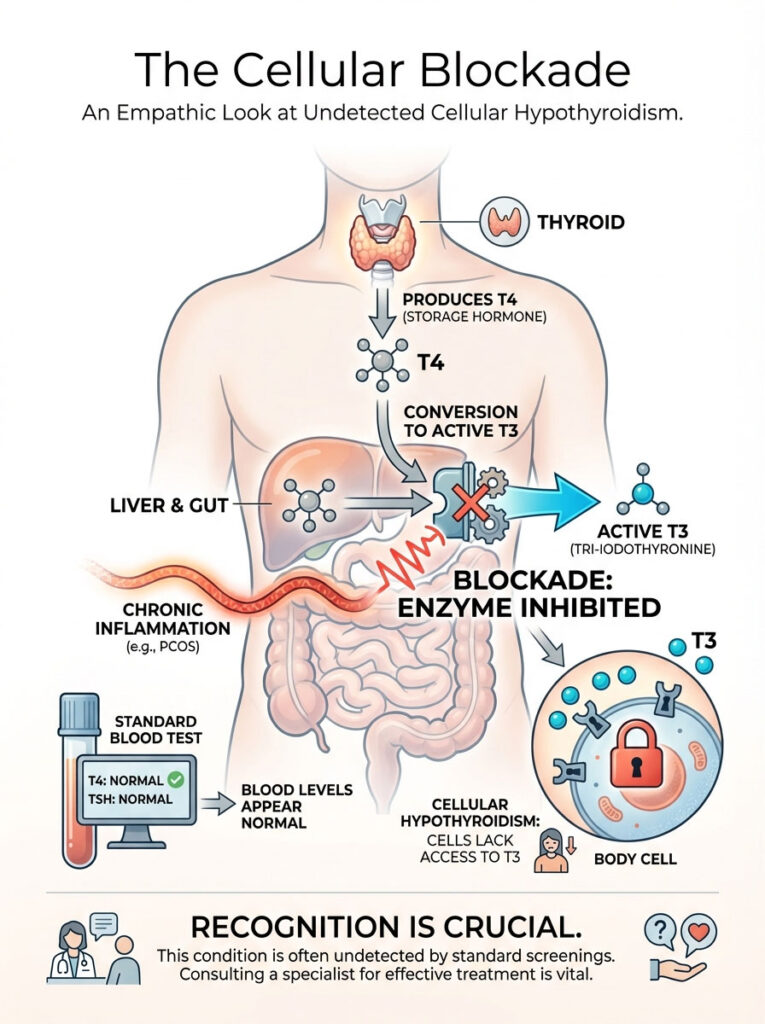
This conversion happens in your liver and gut. However, the chronic inflammation from PCOS shuts down the enzyme required for this magic trick.
Your blood work might show plenty of T4, so your doctor says you are fine. But your cells are starving because they can’t access the active T3.
You are experiencing cellular hypothyroidism, a ghost condition that standard screenings miss.
Eating to Break the Cycle
Food is information. You can signal safety or danger to your glands with every forkful.
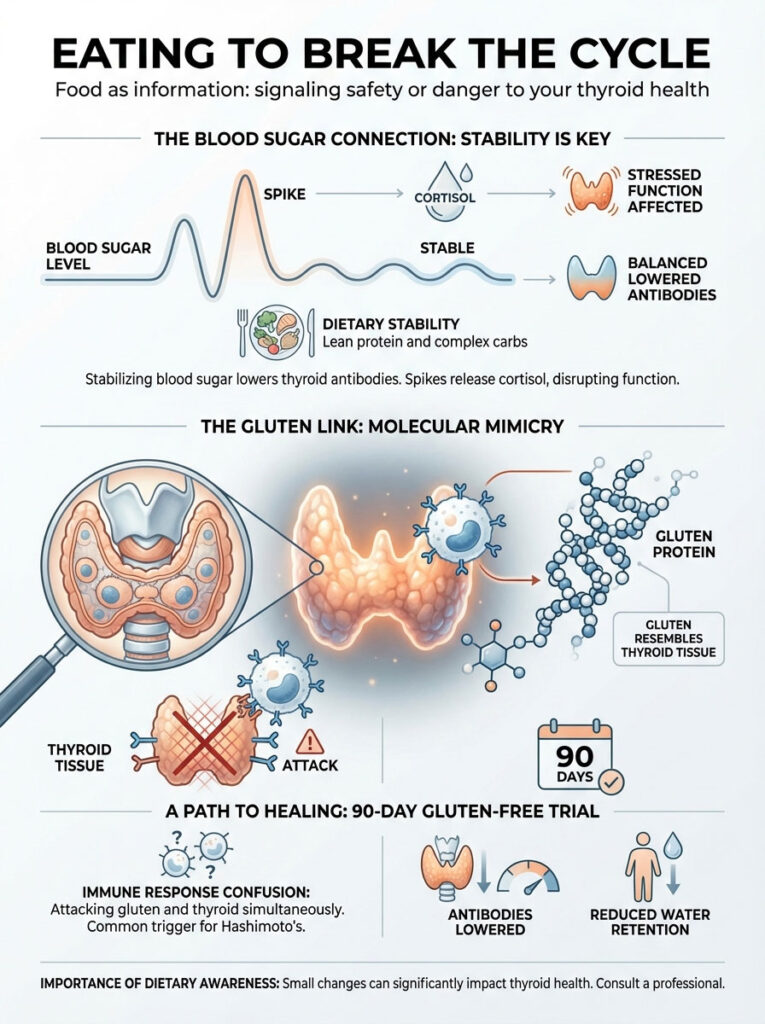
I found that stabilizing blood sugar is the single most effective way to lower thyroid antibodies. When glucose spikes, cortisol follows, and cortisol puts the thyroid to sleep.
The Molecular Mimicry Danger
For my Hashimoto’s patients, gluten is often the enemy. The protein structure of gluten looks suspiciously like thyroid tissue.
When you eat bread, your immune system attacks the gluten. In the confusion, it launches a friendly-fire attack on your thyroid gland.
Going strictly gluten-free for 90 days is often the missing key to lowering antibodies and reducing water retention.
The Fertility Factor
If you are trying to conceive, the stakes are incredibly high. A fetus has no thyroid function for the first 12 weeks.
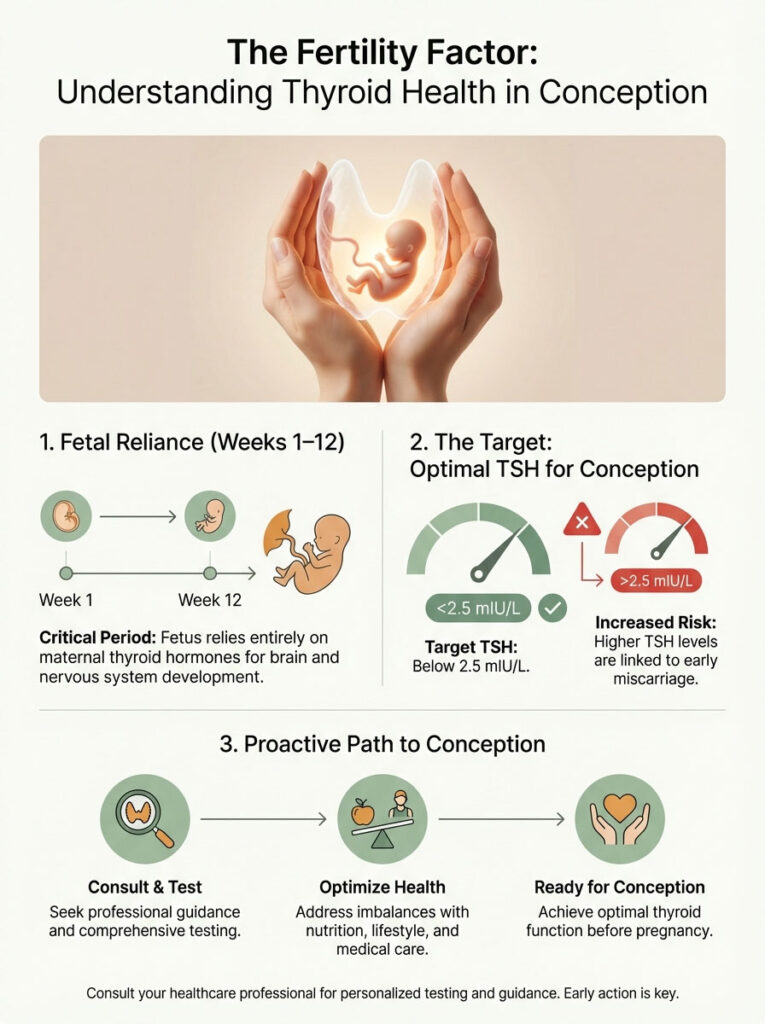
It relies entirely on you. If your tank is empty, the baby’s neural development is at risk.
We strictly aim for a TSH below 2.5 mIU/L for conception. If you are above this number, the risk of early miscarriage increases significantly.
Do not wait until you are pregnant to fix this number. Optimize it now.