Subclinical hypothyroidism (SCH) is a mild thyroid failure where TSH levels are elevated but Free T4 levels are normal. Treatment guidelines are patient-specific. Levothyroxine treatment is strongly recommended if TSH is consistently above 10 mIU/L. For TSH below 10, treatment is considered for patients who are pregnant, trying to conceive, have significant symptoms, or have positive TPO antibodies.
- What is Subclinical Hypothyroidism? Decoding Your Lab Results
- The Symptoms of Subclinical Hypothyroidism: Are You Feeling It?
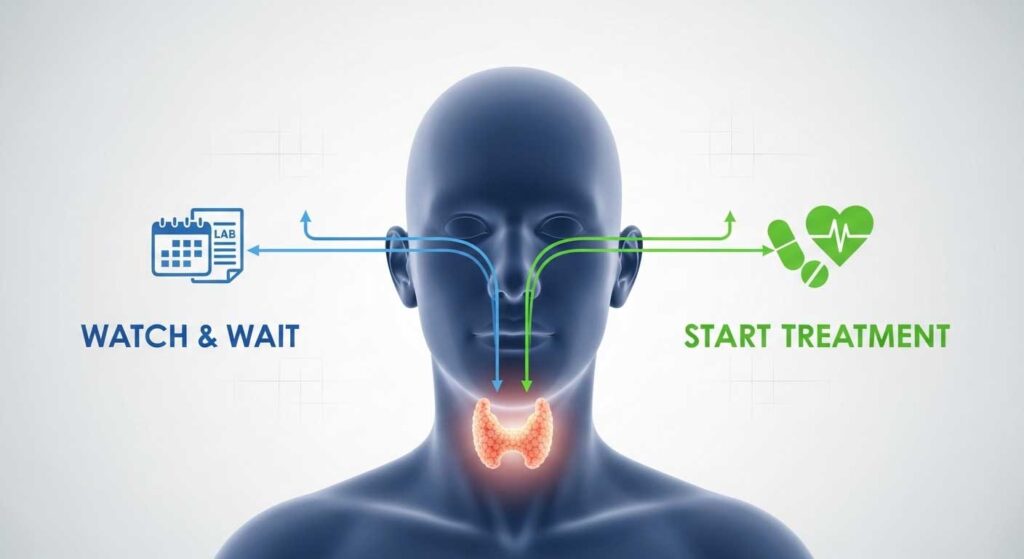
- To Treat or Not to Treat? The Central Question in SCH
- The "Watch and Wait" Approach: Active Observation Explained
- How Subclinical Hypothyroidism is Treated
- Treatment Guidelines for Special Populations
- Weighing the Pros and Cons: A Balanced View on Treatment
- What Happens If Subclinical Hypothyroidism Is Left Untreated?
- Can Diet, Supplements, and Lifestyle Make a Difference?
- Frequently Asked Questions About Subclinical Hypothyroidism Treatment
If you’ve recently been told you have subclinical hypothyroidism, you’re likely feeling a mix of confusion and concern. Your lab results are confusing—one number is “high,” but another is “normal.” Now you’re faced with a critical question: “Do I actually need treatment?” You are not alone in asking this.
This condition is common, but the path forward isn’t always straightforward. The decision to treat involves more than just a lab value; it involves your symptoms, your overall health, your age, and your life goals. This guide will demystify the official subclinical hypothyroidism treatment guidelines, empowering you to have a clear, informed conversation with your doctor about the best approach for you.
What is Subclinical Hypothyroidism? Decoding Your Lab Results
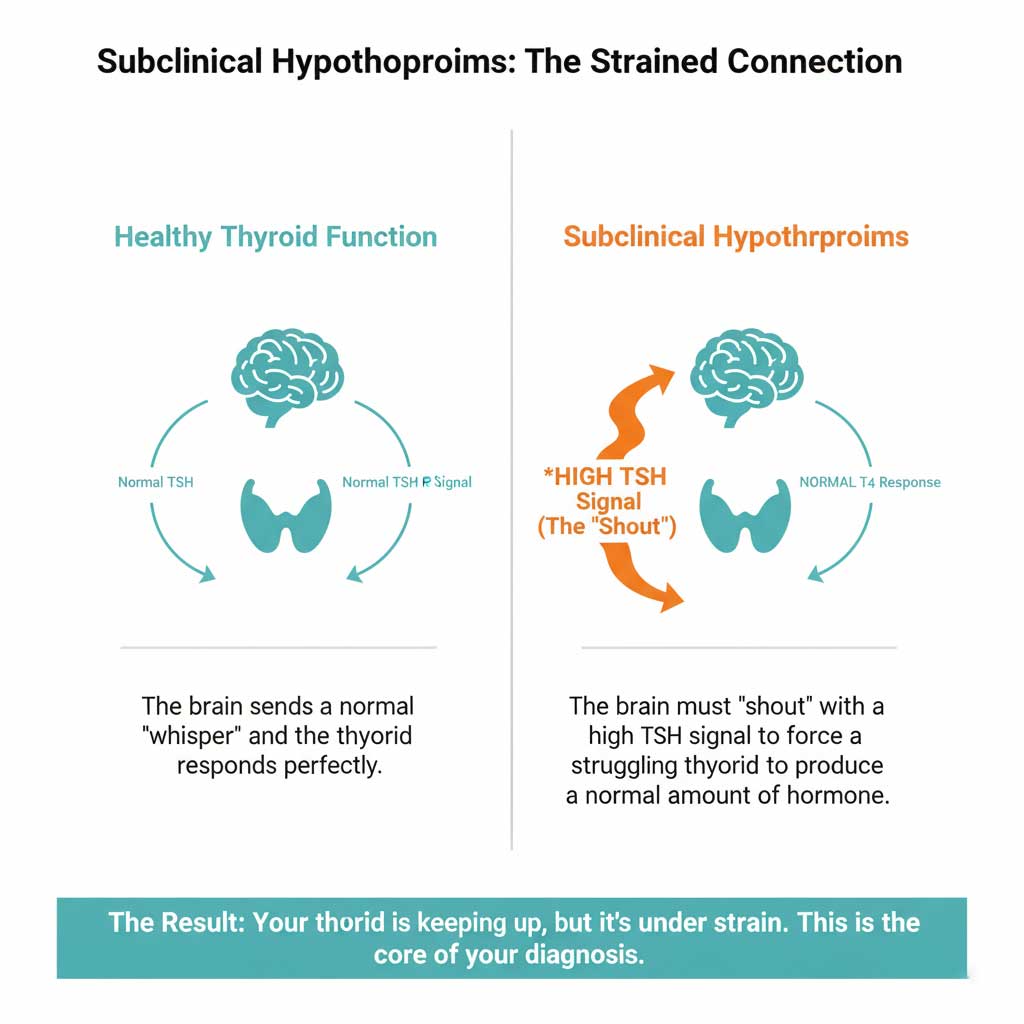
Understanding subclinical hypothyroidism starts with understanding the conversation between your brain and your thyroid gland. Think of it as a thermostat system.
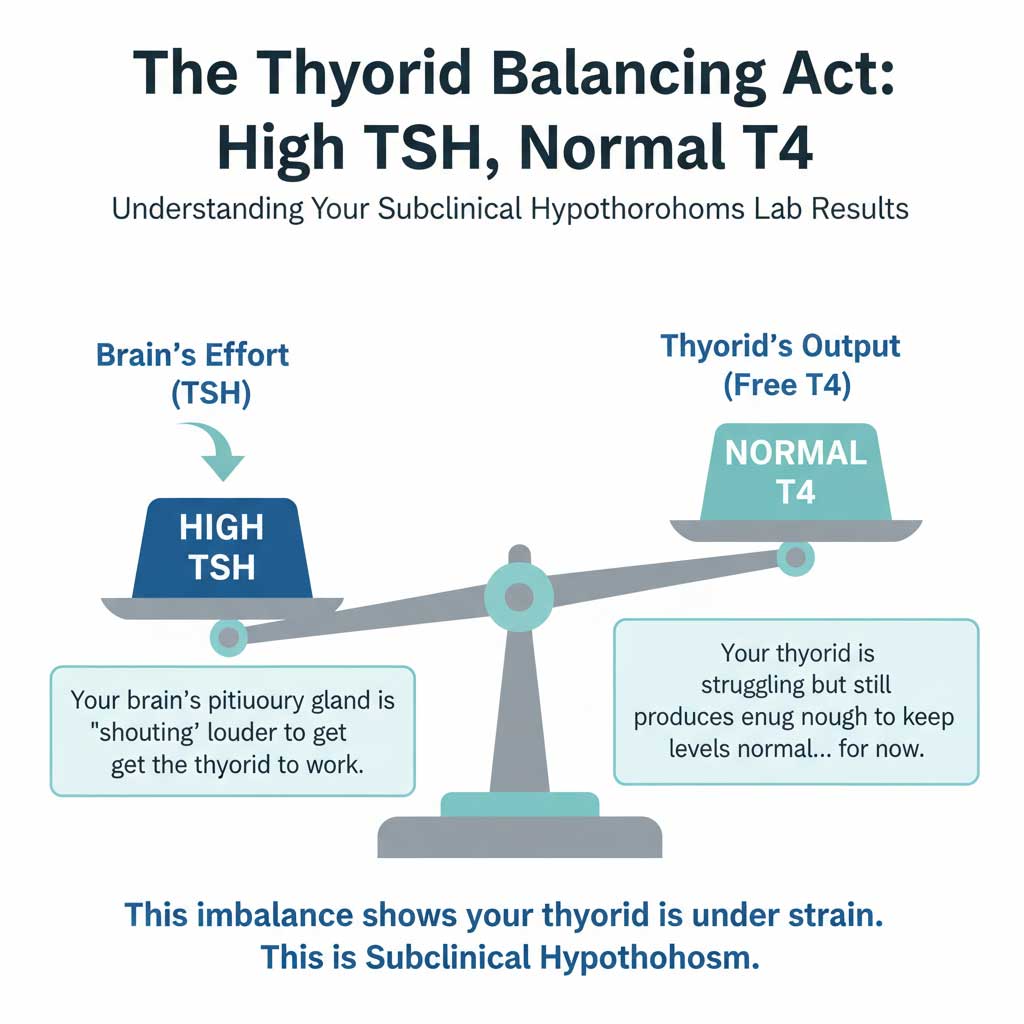
A Simple Definition: High TSH, Normal T4
Your pituitary gland in your brain produces Thyroid-Stimulating Hormone (TSH). TSH acts as a messenger, “telling” your thyroid gland to produce thyroid hormone (like Free T4).
- In a healthy person, the brain sends a normal TSH signal, and the thyroid responds perfectly.
- In subclinical hypothyroidism, your thyroid is slightly underactive and struggling. To compensate, your brain has to “shout” louder by producing more TSH. This high TSH signal is just enough to force your thyroid to produce a normal amount of T4 hormone.
- So, the lab result pattern is a high TSH with a normal Free T4. Your system is working, but it’s under strain.
How is it Different from Overt Hypothyroidism?
The key difference is the Free T4 level. In overt (classic) hypothyroidism, the thyroid is failing more significantly. Even with a very high TSH (a loud shout from the brain), the thyroid cannot produce enough hormone. This results in a high TSH and a low Free T4.
Common Causes and Can It Go Away on Its Own?
The most common cause of subclinical hypothyroidism in the United States is Hashimoto’s thyroiditis, an autoimmune condition where the body’s immune system attacks the thyroid gland. Other causes include aging, a history of thyroid inflammation (thyroiditis), or certain medications.
Interestingly, mild TSH elevations can sometimes be temporary, caused by stress or non-thyroidal illness. For this reason, if your TSH is only slightly high, your doctor will almost always re-test your levels in a few months to see if the elevation is persistent before making a formal diagnosis.
The Symptoms of Subclinical Hypothyroidism: Are You Feeling It?
One of the biggest challenges in diagnosing and deciding on SCH treatment is that the symptoms can be vague, mild, or completely absent. When they do occur, they are the same as those seen in overt hypothyroidism.
Potential symptoms include:
- Persistent fatigue and low energy
- Unexplained weight gain or difficulty losing weight
- Brain fog, poor concentration, and memory issues
- Depression, anxiety, or low mood
- Increased sensitivity to cold
- Constipation and digestive sluggishness
- Dry skin and brittle nails
- Hair loss or thinning
- Elevated cholesterol levels on a lipid panel
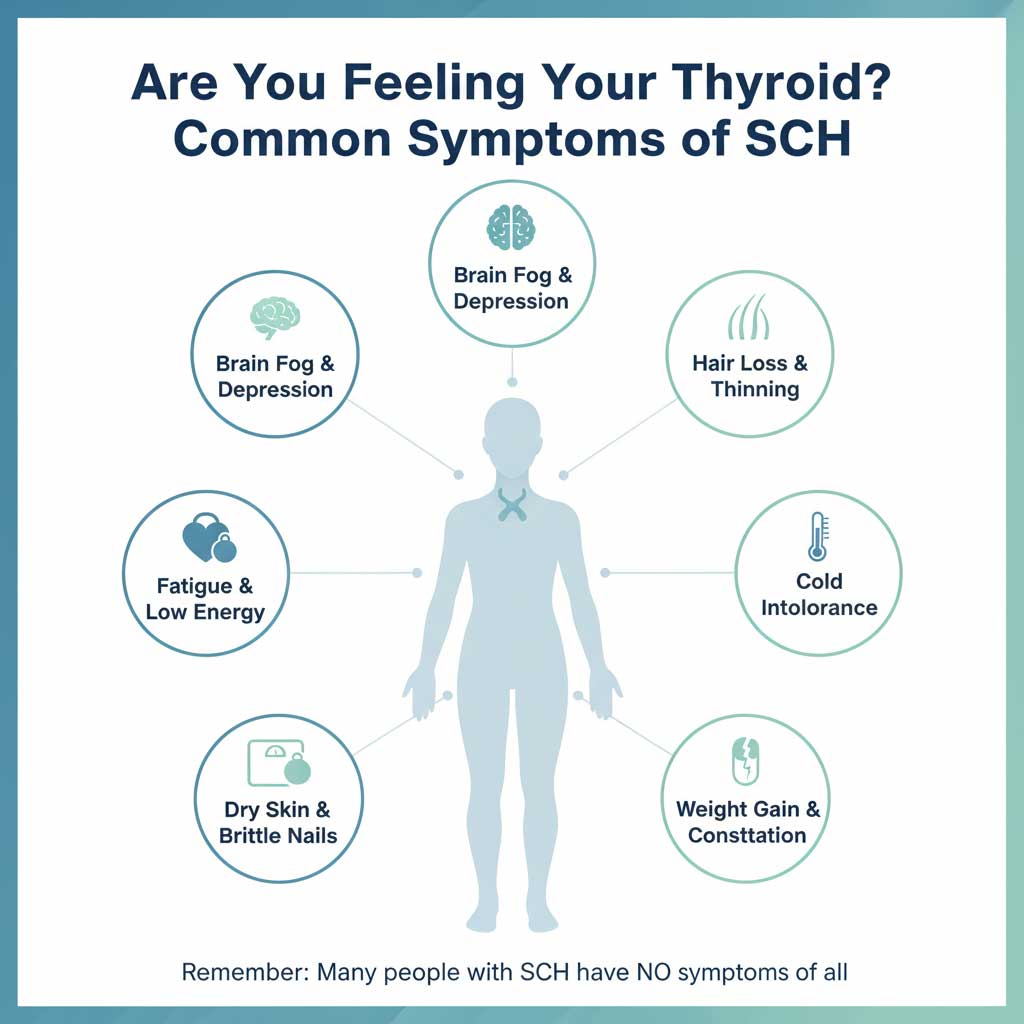
It is crucial to understand that many individuals with a high TSH and normal T4 feel perfectly fine. The absence of symptoms is a major factor that supports the “watch and wait” approach to managing this condition.
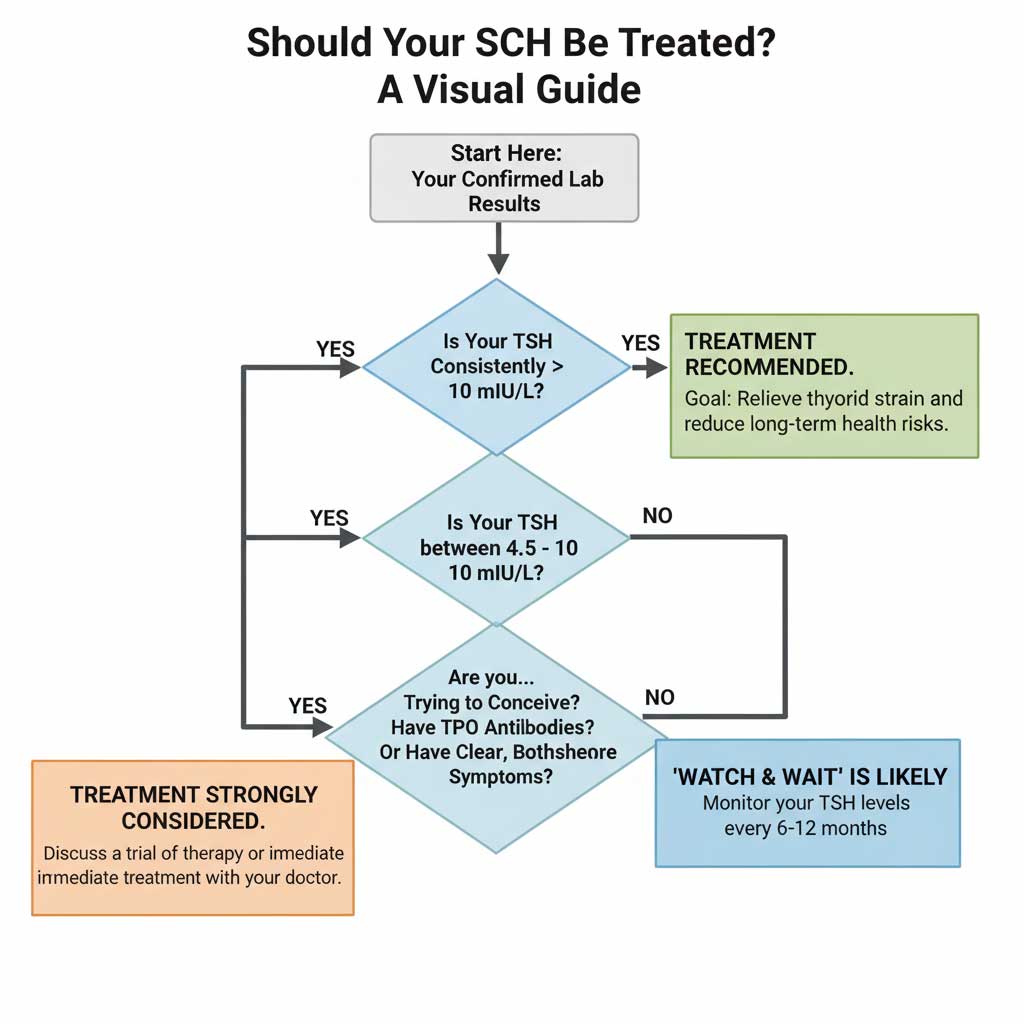
To Treat or Not to Treat? The Central Question in SCH
This is the core of the subclinical hypothyroidism treatment guidelines. The decision is highly individualized and based on a combination of your TSH level, specific risk factors, and personal health situation. The following guide, based on recommendations from leading endocrine organizations like the American Thyroid Association (ATA), can help you understand your doctor’s thought process.
Subclinical Hypothyroidism Treatment Decision Guide (Based on ATA Guidelines)
| Your TSH Level | Key Patient Factors | General Recommendation | Why? |
| TSH > 10 mIU/L | Any patient (regardless of age or symptoms) | Treat with Levothyroxine | High risk of progression to overt hypothyroidism and increased risk of cardiovascular events and heart failure. |
| TSH 4.5 – 10 mIU/L | Trying to Conceive or Pregnant | Treat with Levothyroxine | Untreated SCH is linked to infertility, miscarriage, and negative neurodevelopmental outcomes in the baby. TSH goals are stricter. |
| TSH 4.5 – 10 mIU/L | Positive TPO Antibodies | Strongly Consider Treatment | Indicates underlying Hashimoto’s. Patients have a ~4-5% annual risk of progressing to overt hypothyroidism. Treatment may slow progression. |
| TSH 4.5 – 10 mIU/L | Clear, Bothersome Symptoms | Consider a Trial of Therapy | If a patient has significant symptoms (fatigue, brain fog), a 3-6 month trial of levothyroxine can determine if symptoms improve. |
| TSH 4.5 – 10 mIU/L | High Cholesterol or Heart Disease | Consider Treatment | Thyroid hormone helps regulate lipids. Treatment may help lower LDL cholesterol and improve cardiovascular risk profile. |
| TSH 4.5 – 10 mIU/L | Asymptomatic, TPO Negative, Not Pregnant, Younger than 65-70 | “Watch and Wait” (Observe) | Benefits of treatment may not outweigh the risks. Monitor TSH/T4 every 6-12 months to check for progression. |
| TSH 4.5 – 10 mIU/L | Elderly Patient (>70-75 years old) | Generally Avoid Treatment | TSH normally rises with age. Risks of overtreatment (atrial fibrillation, osteoporosis) often outweigh potential benefits in asymptomatic elderly patients. |
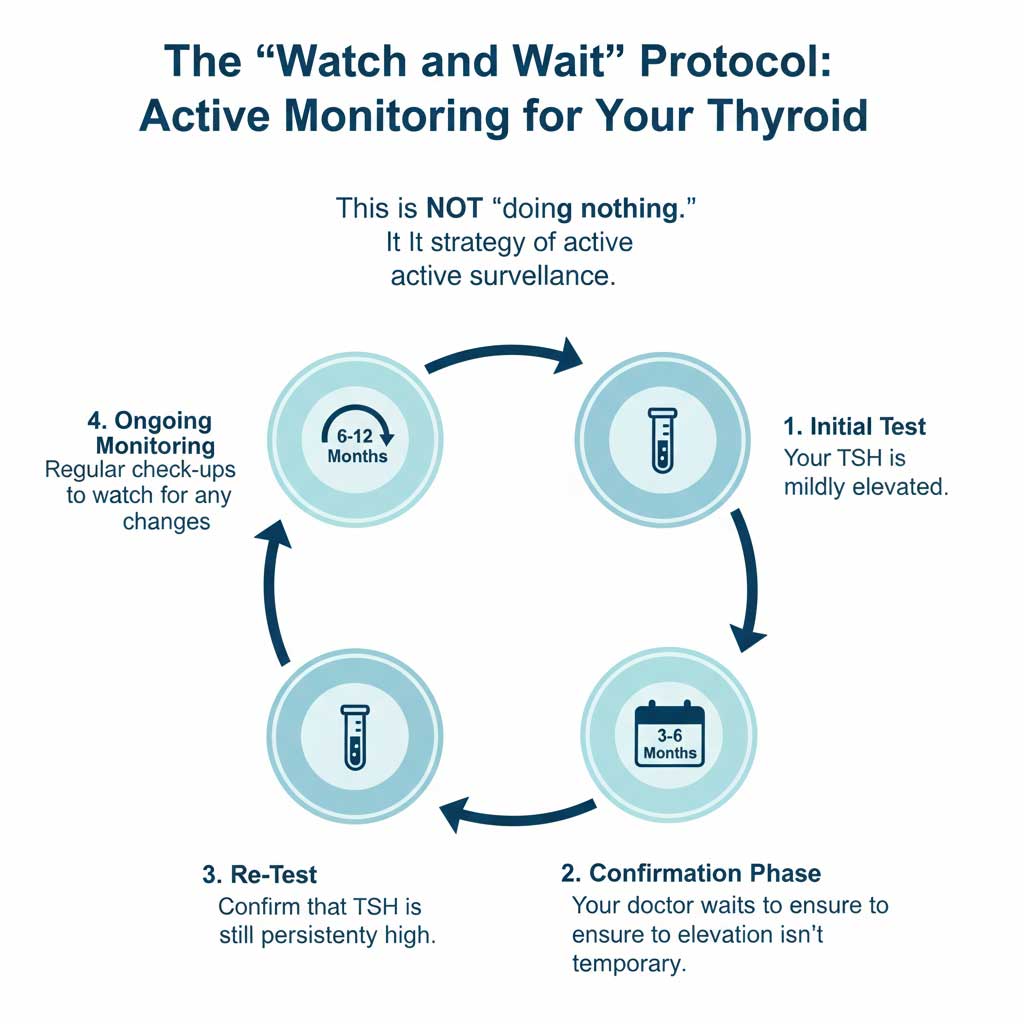
The “Watch and Wait” Approach: Active Observation Explained
For many people with a TSH between 4.5 and 10 mIU/L who are asymptomatic, not pregnant, and younger than 65, the recommended course is “watch and wait.” This is not a passive approach; it is a strategy of active surveillance.
This protocol typically involves:
- Confirmation: Repeating the TSH and Free T4 test in 3 to 6 months to ensure the TSH elevation is persistent and not just a temporary fluctuation.
- Monitoring: If the TSH remains elevated, your doctor will recommend re-checking your thyroid function tests every 6 to 12 months.
- Vigilance: This approach allows you and your doctor to monitor for any new symptoms or significant changes in your TSH level that might shift the balance in favor of starting treatment.
How Subclinical Hypothyroidism is Treated
If the decision is made to begin subclinical hypothyroidism treatment, the process is straightforward and aims to gently restore the body’s hormonal balance.
The Gold Standard Medication: Levothyroxine
The standard treatment is levothyroxine (available as generics and brand names like Synthroid, Levoxyl, and Tirosint). Levothyroxine is a synthetic version of the T4 hormone, molecularly identical to the hormone your own thyroid gland produces. It is a safe, effective, and well-tolerated medication.
Starting Doses and Adjustments
A key principle of SCH treatment is to “start low and go slow.” Because the body is only mildly deficient, a high starting dose is unnecessary and could cause symptoms of over-stimulation. A typical starting dose of levothyroxine for subclinical hypothyroidism is low, often between 25 and 50 micrograms (mcg) per day.
Monitoring and Follow-Up
After starting medication, it takes time for your TSH levels to respond and stabilize. Your doctor will re-check your TSH about 6 to 8 weeks after you begin treatment. Based on that result, your dose may be adjusted up or down as needed. This process is repeated until your TSH is in the optimal range.

What is the Goal TSH Level on Medication?
For most adults being treated for subclinical hypothyroidism, the goal TSH is to bring the level into the lower half of the normal reference range, typically between 0.5 and 2.5 mIU/L. This ensures the thyroid is no longer under strain and can help alleviate symptoms.
Understanding the Risks of Overtreatment
Starting with a low dose is crucial to avoid overtreatment, also known as iatrogenic hyperthyroidism. This occurs when the medication dose is too high, pushing TSH too low and creating an artificial state of an overactive thyroid. Symptoms can include anxiety, heart palpitations, insomnia, and heat intolerance. Over the long term, overtreatment poses serious health risks, especially for older adults, including atrial fibrillation (an irregular heartbeat) and accelerated bone density loss (osteoporosis).
Treatment Guidelines for Special Populations
The standard SCH treatment guidelines are modified for certain groups because their health needs and the risks versus benefits of treatment are different.
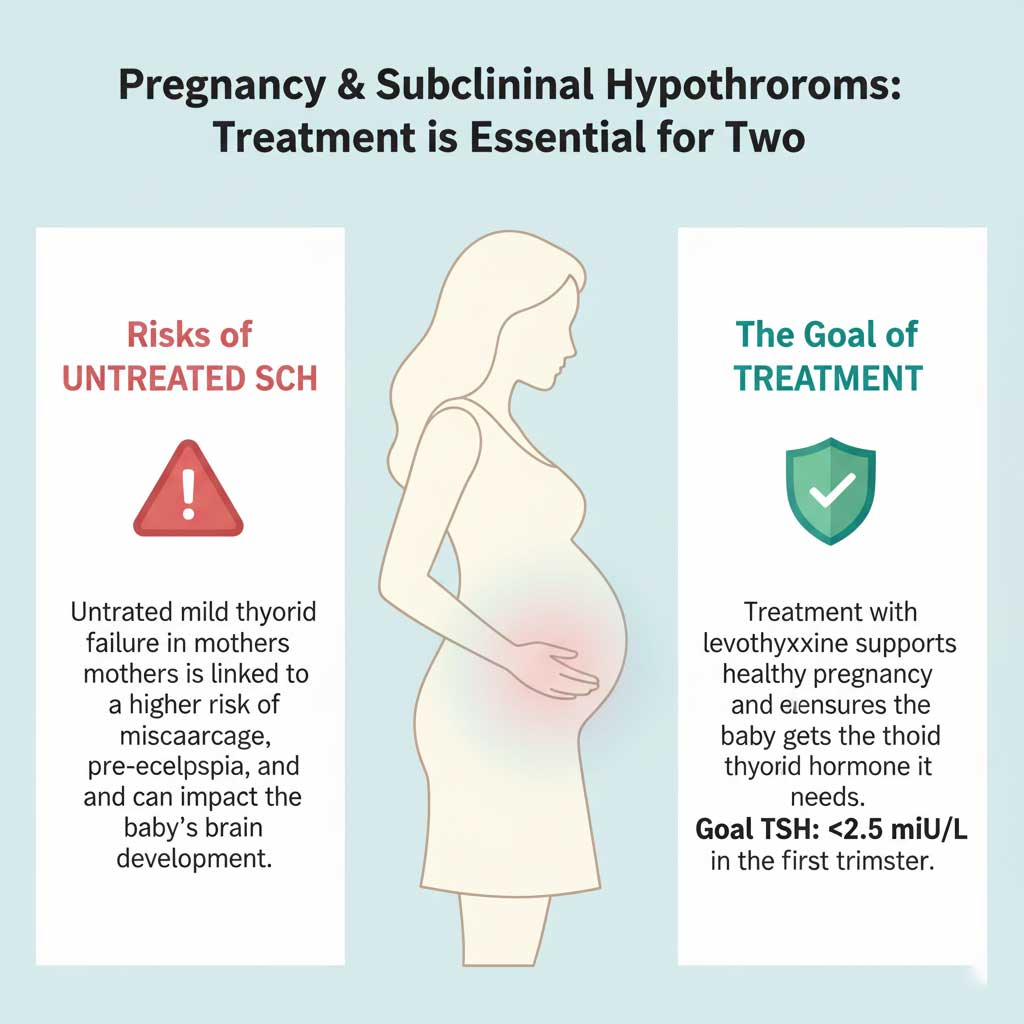
Pregnancy and Fertility: A Critical Time for Treatment
This is the most important exception to the “watch and wait” rule. For women who are pregnant or actively trying to conceive, the subclinical hypothyroidism treatment guidelines are much more aggressive.
- Why? The developing fetus is entirely dependent on the mother’s thyroid hormone for its brain and nervous system development during the first trimester. Even mild maternal thyroid failure has been linked to an increased risk of miscarriage, pre-eclampsia, preterm delivery, and lower IQ in the child.
- Stricter TSH Goals: The TSH goal during pregnancy is much lower, with an ideal TSH of less than 2.5 mIU/L in the first trimester. Treatment is almost always initiated if a woman’s TSH is above this level.
The Elderly (Over 65-70): A More Cautious Approach
At the other end of the spectrum, doctors are far more conservative when considering treatment for subclinical hypothyroidism in older adults.
- Why? TSH levels naturally tend to rise with age. A TSH of 6.0 or 7.0 might be considered normal for a healthy 80-year-old. More importantly, the risks of overtreatment (atrial fibrillation and fractures from osteoporosis) are significantly higher and more dangerous in this population.
- Recommendation: For an older adult with a TSH below 10 and no symptoms, treatment is generally not recommended as the risks often outweigh the potential benefits.

Children and Adolescents
TSH reference ranges vary significantly by age in children. The diagnosis and management of any thyroid condition in a child, including SCH, should always be overseen by a pediatric endocrinologist who can interpret the results in the context of the child’s growth and development.
Weighing the Pros and Cons: A Balanced View on Treatment
The decision of when to treat subclinical hypothyroidism comes down to a careful risk-benefit analysis for each individual.
- Potential Pros: Alleviating bothersome symptoms like fatigue and brain fog, improving cholesterol levels, potentially slowing or preventing the progression to overt hypothyroidism.
- Potential Cons: Committing to daily, lifelong medication; the cost of medication and follow-up lab tests; the risk of side effects or overtreatment if not monitored carefully; and the potential for “medicalizing” a mild condition that might never have caused a problem.
What Happens If Subclinical Hypothyroidism Is Left Untreated?
The primary concern with untreated SCH is its potential to progress to overt hypothyroidism.
The annual risk of this progression is estimated to be between 2% and 5%. However, this risk is not the same for everyone. The risk is significantly higher in individuals who have:
- Positive TPO antibodies (indicating Hashimoto’s disease)
- A higher initial TSH level (e.g., a TSH of 8.5 has a greater chance of progressing than a TSH of 5.5)
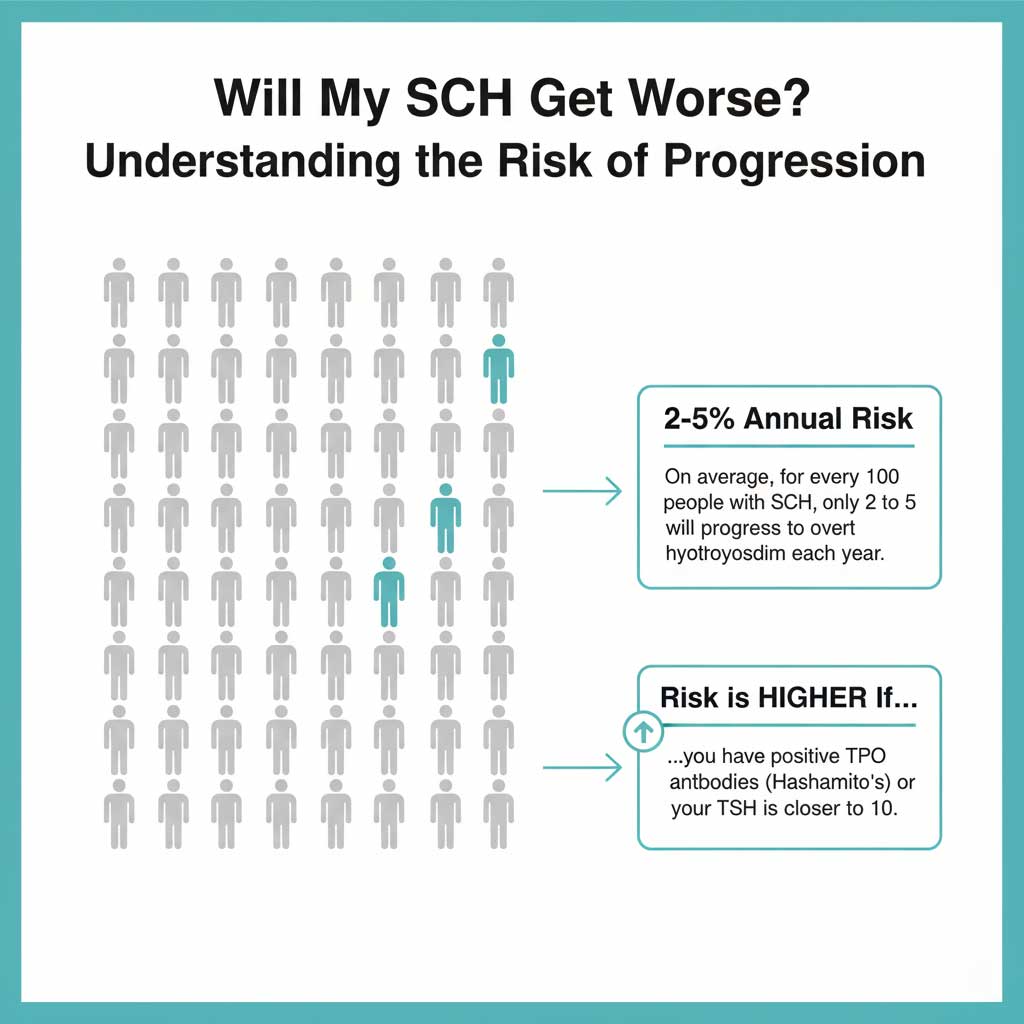
For many people, especially those with a TSH only slightly above the normal range and negative antibodies, the condition may remain stable for years or even a lifetime without ever progressing.
Can Diet, Supplements, and Lifestyle Make a Difference?
While there is no diet that can cure subclinical hypothyroidism, certain nutrients are essential for thyroid health. It’s important to approach this topic with a balanced, evidence-based perspective.
- Iodine: This mineral is a critical building block of thyroid hormone. However, in the U.S., iodine deficiency is rare due to iodized salt. In people with Hashimoto’s, excessive iodine intake can actually worsen the condition.
- Selenium: Some clinical studies suggest that selenium supplementation may help reduce TPO antibody levels in people with Hashimoto’s. However, evidence that it can reverse SCH or prevent its progression is still limited.
- Vitamin D, B12, and Iron: Deficiencies in these nutrients are common, particularly in people with autoimmune conditions like Hashimoto’s. Addressing these deficiencies can help improve overall well-being and energy levels.