Feeling a constant, unshakeable fatigue that coffee can’t fix? Or perhaps you’re finding it harder to catch your breath after a simple flight of stairs. These aren’t just signs of a busy life; they are whispers from your body, and they could be pointing to low hemoglobin. This condition silently affects millions of Americans, masquerading as burnout, stress, or just a normal part of aging.
Table of Contents
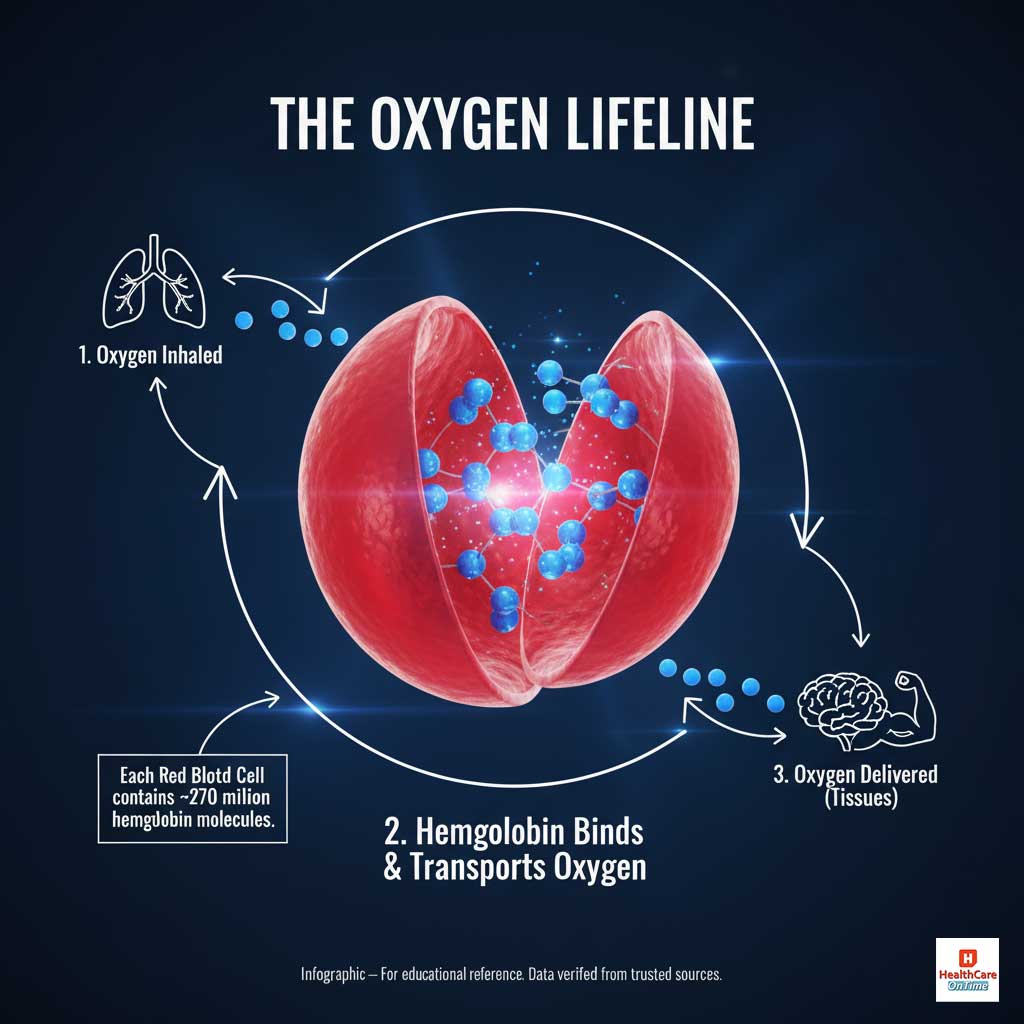
Hemoglobin is the iron-rich protein inside your red blood cells, acting as the body’s dedicated oxygen delivery service. Think of your bloodstream as a vast highway system and your red blood cells as a fleet of delivery trucks. Hemoglobin is the specialized container on each truck, holding the precious cargo—oxygen—that every single cell, tissue, and organ needs to function and thrive. When your hemoglobin levels drop, that delivery fleet shrinks. The result is a body-wide energy crisis that can impact everything from your physical stamina to your mental clarity.
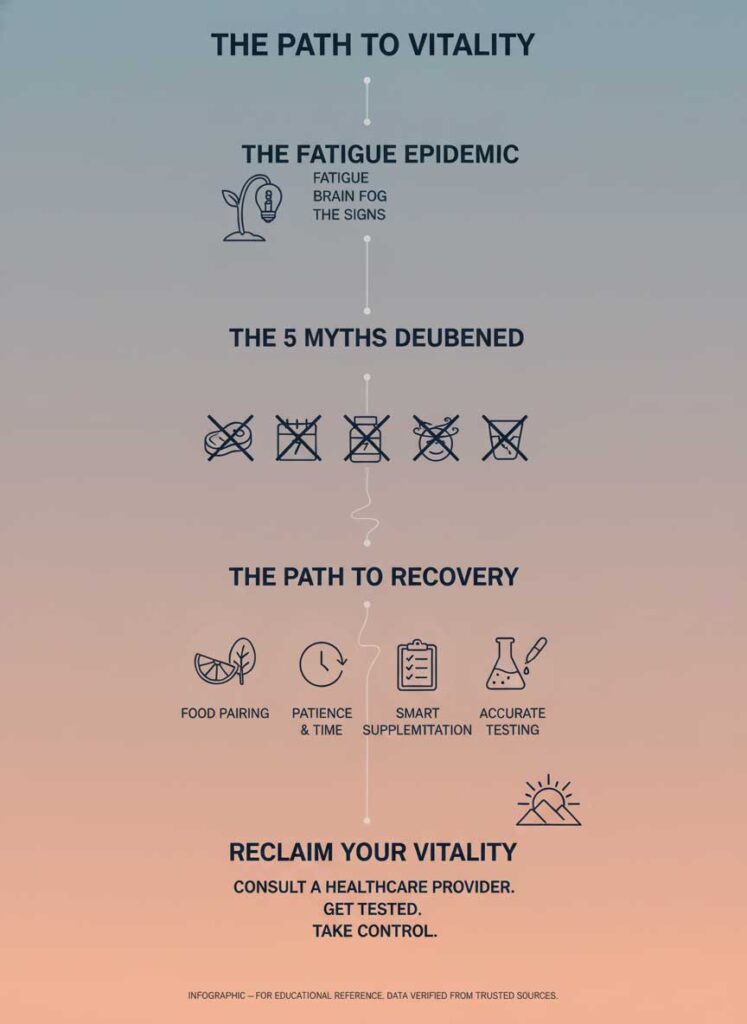
Unfortunately, the path to resolving this is littered with outdated advice and dangerous misinformation. Many common increase hemoglobin myths lead well-intentioned people down ineffective paths, delaying proper care and prolonging their suffering. This is not just another listicle; it’s a deep dive into the science behind hemoglobin. We will dismantle the five most persistent myths with the latest research, provide expert-level strategies, and explore the nuanced low hemoglobin causes. Our goal is to equip you with the knowledge to find the most effective natural ways to boost hemoglobin, understand the best foods to increase hemoglobin, and confidently navigate your journey back to vitality.
Quick Reference: Hemoglobin Myths vs. Facts
Before we dive deep, here is a scannable overview designed to give you a clear picture of the misconceptions versus the scientific reality. This is your starting point for understanding how to raise hemoglobin levels fast and, more importantly, effectively.
| Myth | The Scientific Fact |
| Myth #1: You must eat red meat to raise your hemoglobin. | Fact: Plant-based (non-heme) iron can be highly effective, especially when paired with Vitamin C, which can boost absorption by up to 300%. A diverse diet is key. |
| Myth #2: You can increase your hemoglobin in one week with food. | Fact: Raising hemoglobin and replenishing iron stores is a biological process that takes several weeks to months of consistent, strategic effort. |
| Myth #3: Iron supplements are a simple, universal quick fix. | Fact: The effectiveness of supplements depends heavily on the type, dosage, timing, and your body’s unique ability to absorb them, which can be hindered by many factors. |
| Myth #4: The only signs of low hemoglobin are paleness and dizziness. | Fact: The symptoms are vast and often subtle, including fatigue, brain fog, anxiety, hair loss, and poor athletic performance—some of the most common signs of low iron in women. |
| Myth #5: Dehydration has no effect on hemoglobin test results. | Fact: Dehydration concentrates your blood, leading to a falsely high hemoglobin reading that can mask a serious underlying deficiency, delaying diagnosis and treatment. |
Myth #1: “All Red Meat Is the Ultimate and Only Hemoglobin Booster”
This is perhaps the most deep-rooted belief about boosting hemoglobin. The idea that a daily steak is the one-and-only powerful anemia treatment at home comes from a place of truth: red meat is an exceptional source of heme iron. However, declaring it the only solution is not only inaccurate but also excludes millions of people and ignores the sophisticated science of nutrient absorption.
The Scientific Reality: A Deeper Look at Heme vs. Non-Heme Iron
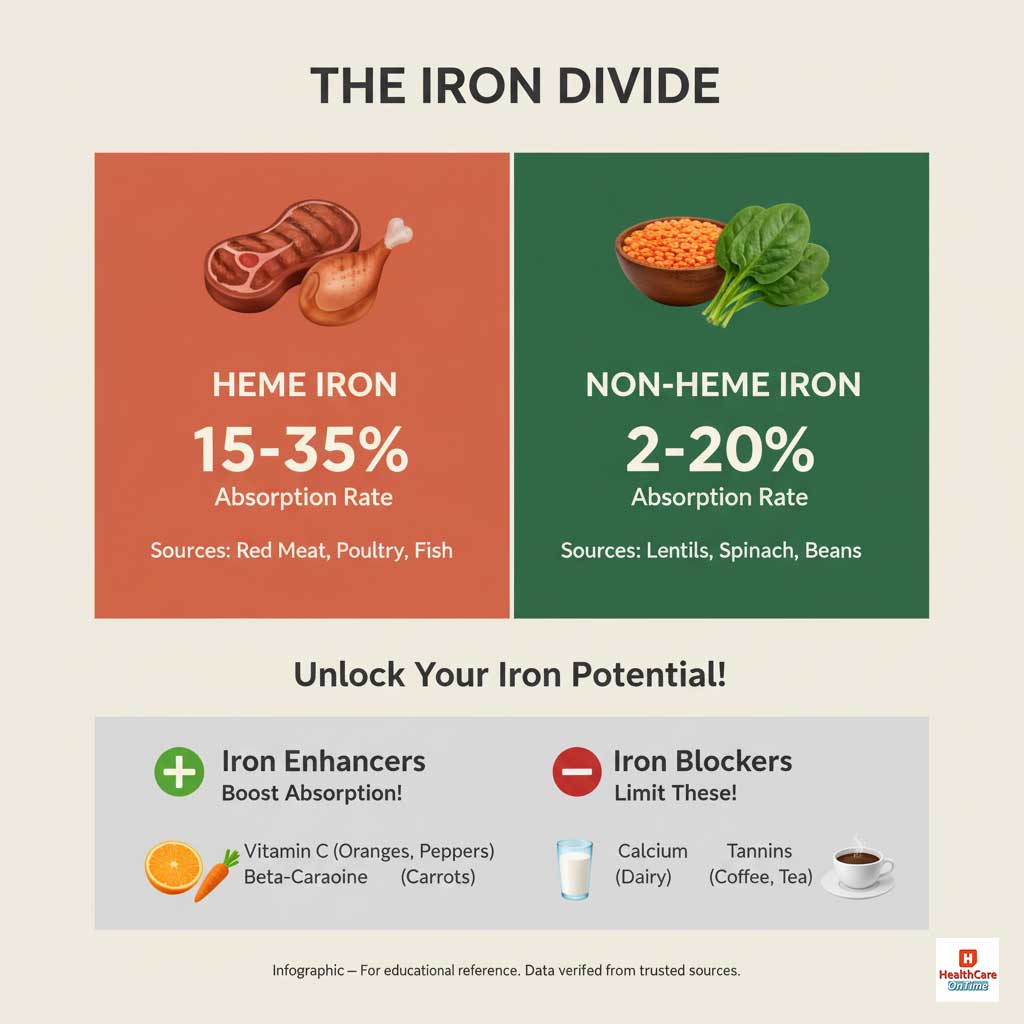
To truly understand iron, you must know its two forms. This knowledge is crucial for debunking the persistent myths about plant-based iron absorption.
- Heme Iron: This form is found exclusively in animal flesh and blood—think red meat, poultry, and fish. Its structure allows it to be absorbed directly by special receptors in your intestines, making it highly bioavailable. Your body typically absorbs between 15% and 35% of the heme iron you consume.
- Non-Heme Iron: This is the form of iron found in all plant-based foods—lentils, spinach, tofu, beans, and fortified cereals. Its absorption is a more complex process, with rates varying from 2% to 20%. This doesn’t mean it’s inferior; it just means it’s more sensitive to the other foods you eat with it.
Furthermore, hemoglobin production is a team sport. It’s not just about iron. The relationship between Vitamin B12 and hemoglobin is critical, as B12 is essential for producing healthy red blood cells. Likewise, many folate-rich foods for anemia, such as leafy greens, asparagus, and legumes, are plant-based powerhouses. Focusing solely on meat means you might miss out on these other vital nutrients.
Actionable Strategy: Becoming an Iron Absorption Expert
Instead of just eating more iron, the goal is to absorb more of the iron you eat. You can transform your meals into high-efficiency iron-delivery systems by mastering food pairing. This means strategically combining “iron enhancers” with your meals and separating them from “iron blockers.” Here’s a detailed guide on how to do it.
| Nutrient Interaction | Actionable Strategy & Examples | Why It Works |
| Enhancer: Vitamin C | Pair iron-rich foods with sources of Vitamin C. Squeeze lemon on spinach salad; add bell peppers to a bean chili; have a side of kiwi with your fortified cereal. | Vitamin C is a powerful antioxidant that converts non-heme iron into a form that is much more easily absorbed by your body. |
| Enhancer: Beta-Carotene | Combine iron sources with foods rich in beta-carotene. Think sweet potatoes with black beans, or kale and carrots in a lentil soup. | Beta-carotene (a precursor to Vitamin A) has been shown to form a complex with iron, preventing it from being bound by absorption inhibitors. |
| Blocker: Calcium | Avoid consuming high-calcium foods (milk, yogurt, cheese) or calcium supplements at the same time as your main iron-rich meal. Separate them by at least two hours. | Calcium competes with iron for the same absorption pathways in the gut. When taken together, calcium almost always wins, reducing iron uptake. |
| Blocker: Polyphenols | Drink your coffee or black tea at least one hour before or two hours after your iron-rich meal, not with it. The same applies to red wine. | These compounds, also called tannins, bind with iron in the digestive tract, forming an insoluble compound that your body cannot absorb. |
| Blocker: Phytates | Soak, sprout, or ferment legumes, whole grains, and nuts before eating them. This reduces their phytic acid content. | Phytates are anti-nutrients that bind to minerals like iron, zinc, and magnesium, preventing their absorption. |
Myth #2: “You Can Naturally Increase Hemoglobin in a Week”
When you feel profoundly tired, the desire for immediate relief is overwhelming. This desperation fuels the search for “how to increase hemoglobin in a week naturally.” While making positive dietary changes can certainly make you feel better by providing a rush of nutrients, expecting a measurable, significant rise in your hemoglobin count in just seven days is biologically improbable.
The Biological Reality: The Patient Pace of Red Blood Cell Production
Your body is a remarkable factory, but it cannot be rushed. The complex, multi-step process of creating new, mature red blood cells is called erythropoiesis. This journey begins in your bone marrow and is governed by hormones and the availability of raw materials—namely iron, Vitamin B12, and folate.

According to leading hematology resources and the National Heart, Lung, and Blood Institute (NHLBI), it takes several weeks of consistent, targeted intervention for your bone marrow to produce enough new, healthy red blood cells to make a meaningful impact on your overall hemoglobin levels. Understanding this timeline is one of the most vital natural ways to boost hemoglobin because it sets realistic expectations and encourages consistency over short-term, ineffective sprints.
Case Study: The Misdiagnosis of Burnout
Consider the real-world experience of a 42-year-old teacher who felt utterly depleted. For nearly a year, she and her doctor attributed her exhaustion, brain fog, and irritability to the high-stress nature of her job—a classic case of suspected burnout. She tried vacations, meditation, and reducing her workload, but nothing touched the deep, cellular fatigue. These were all subtle iron deficiency anemia symptoms hiding in plain sight.
It was only when she developed restless legs at night and significant hair shedding that a more thorough investigation was launched. A blood panel revealed a shockingly low ferritin (stored iron) level of 8 ng/mL and a hemoglobin of 9.5 g/dL. Her recovery was not a one-week fix. It was a six-month, doctor-guided journey involving high-dose supplements and a radical dietary overhaul. Her story is a powerful testament that true recovery requires patience and correctly identifying the underlying low hemoglobin causes.
Myth #3: “Iron Supplements Are a Simple, Foolproof Solution”
When diet alone isn’t cutting it, iron supplements often seem like the logical next step. They are frequently viewed as a simple pill to solve a complex problem, a direct route to raise hemoglobin levels fast. While supplements are a cornerstone of an effective anemia treatment at home for millions, believing they are a universally foolproof solution is a dangerous oversimplification.

The Reality: Navigating Absorption, Side Effects, and Root Causes
The critical question, “Do iron supplements really work for anemia?” has a more complicated answer than a simple yes or no. Their success is contingent on a host of factors that are often ignored.
- The Form of Iron Matters: Not all supplements are created equal. The most commonly prescribed form, ferrous sulfate, is effective but notorious for causing gastrointestinal side effects. Gentler, more modern forms like iron bisglycinate chelate are often better tolerated and absorbed, but may be more expensive.
- The Battle in Your Gut: As discussed, what you take with your iron is critical. A supplement taken with a glass of milk or a cup of coffee is often rendered useless.
- Underlying Absorption Issues: Sometimes, the problem isn’t a lack of intake but a malfunction in the absorption machinery itself. This is particularly true for individuals with undiagnosed or poorly managed celiac disease, Crohn’s disease, or even a common stomach bacteria called H. pylori. These conditions can cause inflammation and damage to the intestinal lining where iron is absorbed.
Actionable Strategy: A Smarter Approach to Supplementation
- Demand a Full Panel: Before starting any supplement, insist on a comprehensive blood test that includes not just hemoglobin but also ferritin (iron stores), serum iron, TIBC (total iron-binding capacity), and transferrin saturation. This gives a complete picture of your iron status.
- Start Low and Go Slow: If you are sensitive, ask your doctor about starting with a lower dose or taking it every other day. Recent research suggests that alternate-day dosing can actually improve absorption and reduce side effects by lowering levels of hepcidin, the hormone that blocks iron absorption.
- Optimize Your Timing: For maximum absorption, take your iron supplement on an empty stomach. If this causes nausea, try taking it with a small amount of food that does not contain calcium, phytates, or tannins—a handful of strawberries is a perfect choice.
- Consider the Co-Factors: Ensure your diet is also rich in Vitamin B12 and folate. Taking iron without these essential partners is like trying to build a car with only the frame; you need all the parts for it to function.
Myth #4: “If You’re Not Pale or Dizzy, Your Hemoglobin Is Normal”
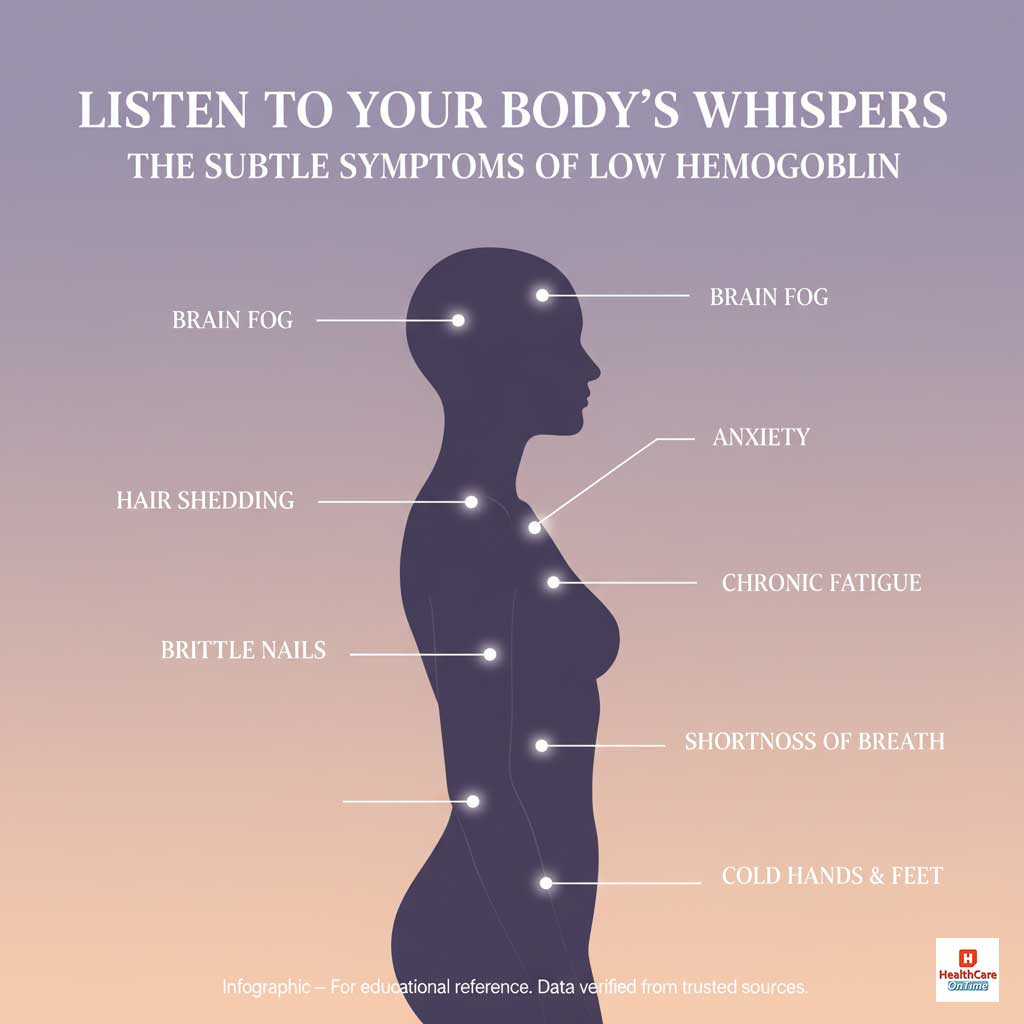
When we picture anemia, our minds often conjure an image of a frail, pale, and dizzy individual. While these are certainly classic symptoms of severe, advanced anemia, they represent only the final act of the play. Relying solely on these dramatic signs means you could be ignoring the subtle prologue and early chapters where intervention could be far easier and more effective.
The Reality: The Wide and Varied Language of Low Hemoglobin
The first signs of low hemoglobin are rarely dramatic. They are often a collection of subtle, nagging symptoms that can be easily dismissed or misattributed to something else. Recognizing this broader spectrum of iron deficiency anemia symptoms is the key to early detection.
This is a more comprehensive checklist of symptoms to watch for:
- Profound Fatigue: A deep, persistent weariness that sleep doesn’t resolve.
- Cognitive Impairment: Brain fog, difficulty concentrating, memory lapses, and reduced mental sharpness.
- Emotional & Mood Changes: Increased anxiety, unexplained irritability, or feelings of depression.
- Physical Signs: Noticeable hair shedding, brittle or spoon-shaped nails, cracks at the corners of your mouth (angular cheilitis), and a sore or swollen tongue.
- Energy & Circulation Issues: Shortness of breath with minimal exertion (like walking up stairs), cold hands and feet, and restless leg syndrome at night.
The signs of low iron in women can be particularly telling. Menorrhagia, or heavy menstrual bleeding, is one of the leading low hemoglobin causes in premenopausal women, creating a vicious cycle of monthly iron loss that is difficult to overcome with diet alone.
Case Study: The Athlete’s Paradox
Let’s revisit the female long-distance runner. Her story is a perfect example of the “athlete’s paradox.” She was incredibly fit, ate a nutrient-dense diet, and looked the picture of health. Yet, her performance plummeted. She was experiencing “runner’s anemia,” a condition caused by a combination of increased iron demands from strenuous exercise, iron loss through sweat, and minor gastrointestinal bleeding that can occur during intense runs. Her primary symptom wasn’t paleness; it was an inability to perform at her peak. This highlights that for many, the first sign of a problem is a functional decline, not a visible one.

Myth #5: “Dehydration and Hemoglobin Levels Are Unrelated”
You go for a routine physical, you haven’t had much to drink that morning, and your lab report comes back. Your hemoglobin level is smack in the normal range. You receive a clean bill of health, but this result could be a dangerous illusion. One of the most critical and least understood factors that can influence a blood test is your hydration status.
The Scientific Reality: The Masking Effect of Hemoconcentration
The concept that dehydration can cause low hemoglobin readings to appear falsely normal is rooted in a simple principle: hemoconcentration. As we’ve discussed, your blood is a mixture of cells and plasma. When you are dehydrated, the water content in your plasma drops significantly.
This doesn’t change the number of red blood cells you have, but it decreases the total volume of your blood. Consequently, the red blood cells become more concentrated. Since a lab test measures the concentration of hemoglobin in a given sample of blood, this artificially dense sample will yield a higher—and potentially misleading—result. This can mask a genuine iron deficiency, giving both you and your doctor a false sense of security and delaying critical treatment.
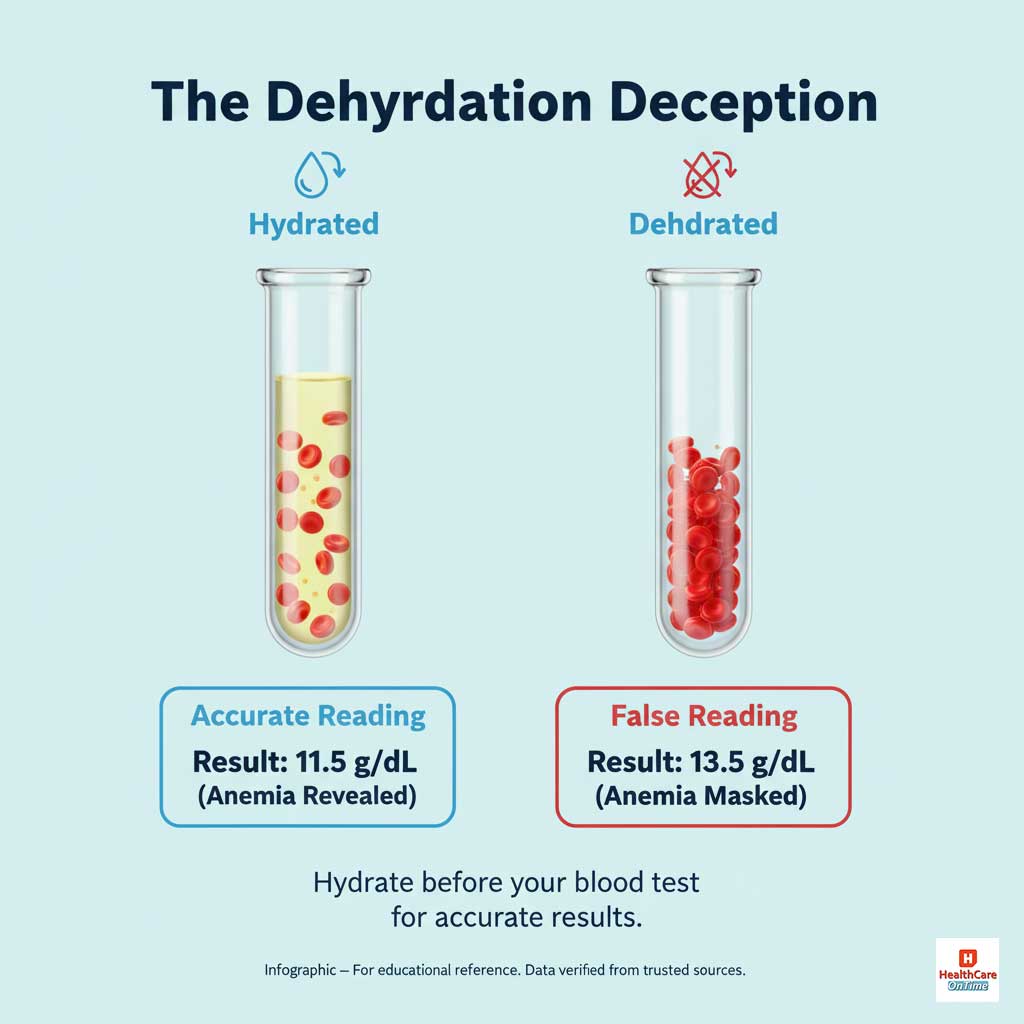
Actionable Strategy: How to Prepare for an Accurate Blood Test
- Hydrate for 24 Hours: Your preparation shouldn’t start the morning of the test. Make a concerted effort to drink plenty of water throughout the day before your blood draw.
- Morning Hydration is Key: Drink one or two full glasses of water upon waking on the day of your test.
- Be Transparent with Your Doctor: Always discuss your results in context. Mention if you were rushing, had just exercised, or feel you may have been dehydrated. A good clinician will take this information into account when interpreting your lab values.
Final Summary & Key Takeaways
The journey to restoring healthy hemoglobin levels is one of science, strategy, and self-awareness. It requires moving beyond simplistic and outdated increase hemoglobin myths and embracing a more nuanced understanding of your body. By doing so, you can replace confusion with confidence and fatigue with vibrant energy.
Here are the five foundational truths to guide your path:
- Dietary Diversity is Non-Negotiable: A rich, varied diet containing both plant-based and animal-based foods to increase hemoglobin provides the full spectrum of nutrients your body needs.
- Biology Has Its Own Timeline: Be patient. True recovery is a marathon, not a sprint. Celebrate small improvements and trust the process.
- Supplements Are a Targeted Tool: Use them wisely and under the guidance of a healthcare professional to address the root low hemoglobin causes, not just the symptoms.
- Become a Symptom Detective: Listen to your body’s subtle whispers. The first signs of low hemoglobin are rarely a shout.
- Data Integrity Matters: Ensure your diagnostic tests are as accurate as possible by being properly hydrated. A correct diagnosis is the bedrock of any successful treatment plan.

Stop guessing and start investigating. Empower yourself with knowledge, work with a trusted healthcare provider, and take deliberate, informed steps. By debunking these myths, you can finally clear the path to reclaiming the boundless energy and vitality you deserve.
Frequently Asked Questions (FAQs)
What is a dangerously low hemoglobin level?
While normal ranges vary, a hemoglobin level below 7.0 to 8.0 grams per deciliter (g/dL) is generally considered dangerously low and may require urgent medical intervention like a blood transfusion. It’s critical to discuss any low reading with your doctor.
Can I raise my hemoglobin in 7 days?
While you can start improving your iron intake immediately, it is biologically impossible to see a significant, lasting increase in your hemoglobin count in just one week. Building new red blood cells and replenishing iron stores is a gradual process that takes several weeks to months.
What are the 3 main causes of anemia?
The three primary low hemoglobin causes are: 1) Blood loss (either acute from an injury or chronic from conditions like heavy periods or ulcers), 2) Decreased or faulty red blood cell production (most often due to deficiencies in iron, Vitamin B12, or folate), and 3) Increased destruction of red blood cells (a condition known as hemolytic anemia).
Is 10.5 hemoglobin low?
Yes, a hemoglobin level of 10.5 g/dL is considered moderately low for both adult men and non-pregnant women. It indicates a clear state of anemia that requires medical evaluation to determine the underlying cause and the most effective treatment plan.
Does drinking a lot of water increase hemoglobin?
No, drinking water does not directly create more hemoglobin. However, being properly hydrated ensures your blood volume is normal, which is essential for an accurate blood test. Dehydration can cause low hemoglobin readings to appear falsely high, masking a real problem.
What are the symptoms of low hemoglobin in females?
Common symptoms of low hemoglobin in females are often widespread and include chronic fatigue, heavy menstrual bleeding, shortness of breath, headaches, anxiety, hair thinning, brittle nails, and cold hands and feet.
Which fruit is best for hemoglobin?
The best fruits to increase hemoglobin levels quickly are those rich in Vitamin C, as they enhance iron absorption. While pomegranates are often cited, citrus fruits, strawberries, kiwi, and bell peppers (botanically a fruit) are all excellent choices to eat alongside iron-rich foods.
What is the fastest way to cure anemia?
The fastest and most effective way to raise hemoglobin levels fast and resolve anemia is to follow a plan from a healthcare provider. For severe deficiencies, this may involve intravenous (IV) iron infusions, which bypass the gut for 100% absorption, delivering iron directly to your bloodstream.
Do iron supplements really work for anemia?
Yes, when used correctly, iron supplements are a highly effective treatment for iron deficiency anemia. Their success depends on the right dosage, the right form of iron for your body, and a strategy to maximize absorption and minimize side effects.
What foods block iron absorption?
The main culprits that block iron absorption are calcium-rich foods (dairy), polyphenols/tannins (in coffee, tea, and red wine), and phytates (in whole grains, legumes, and nuts). It’s best to separate these from your main iron-rich meals by at least two hours.
Can you have low iron but normal hemoglobin?
Yes, absolutely. This is the first stage of iron deficiency, known as “iron deficiency without anemia.” It means your body’s iron stores (ferritin) are depleted, but you are still managing to produce enough hemoglobin. You can still experience significant symptoms like fatigue and brain fog in this stage.
Why is my hemoglobin low even though I eat meat?
This is a common and important question. It could be due to several factors: chronic blood loss that outpaces your intake (e.g., from a gastrointestinal issue), an underlying medical condition that impairs iron absorption (like celiac disease or low stomach acid), or consuming too many iron blockers with your meals. It highlights the need for a thorough medical investigation.









