Receiving a lab order from your doctor often brings an immediate wave of uncertainty. The most common question is a simple one, yet it causes significant confusion: “Can I eat before a blood test?” For decades, fasting has been a standard instruction, but as diagnostic science evolves, so do the guidelines. The modern wellness trend is toward patient empowerment, which starts with understanding your own health data and the simple steps required to get accurate results.
Table of Contents
This guide provides a comprehensive, evidence-based answer to that critical question: which blood tests can be done without fasting? While some tests absolutely require an empty stomach for accuracy, a surprising number of non-fasting blood tests are available. We will deliver a clear breakdown of which tests fall into which category, explore the science behind these rules, and provide actionable tips to help you prepare for your next lab appointment with absolute confidence. Understanding the requirements for your specific no fasting blood work is the first step toward taking control of your health journey.
The Core Concept: What Does “Fasting for a Blood Test” Actually Mean?
Before we explore the extensive list of non-fasting blood tests, it’s essential to understand the medical definition of fasting and why it’s a critical instruction for certain types of lab work. This clarity helps remove ambiguity and ensures you are properly prepared.
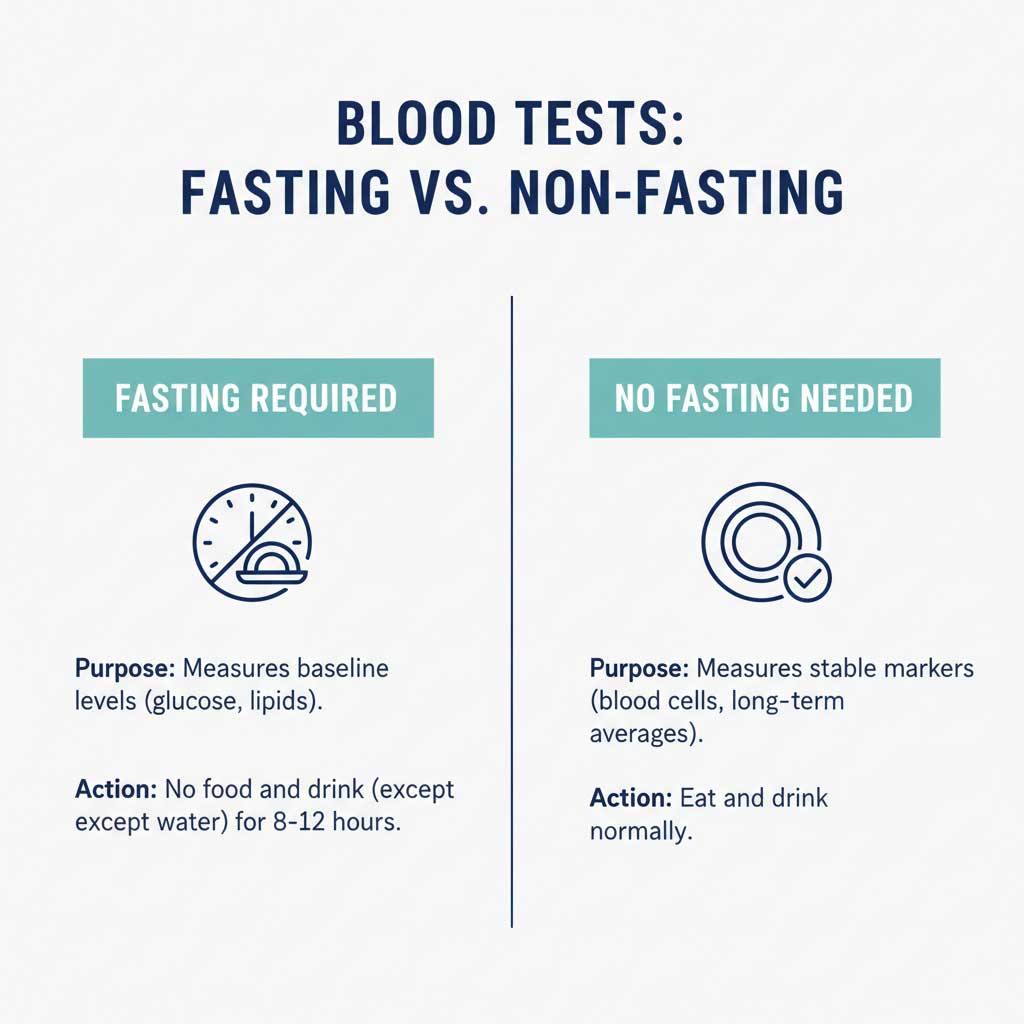
Defining Medical Fasting
When your healthcare provider instructs you to fast, it means you must abstain from all food and most drinks for a specific period, typically between 8 and 12 hours. While you are usually encouraged to drink plain water to stay hydrated, other beverages like coffee, tea, juice, and soda are strictly off-limits.
This instruction is not arbitrary. When you eat and drink, your body breaks down the contents into nutrients like glucose, lipids (fats), proteins, and minerals, which are then absorbed into your bloodstream. This process can temporarily, yet significantly, elevate the levels of these substances, creating a metabolic “noise” that can interfere with test results.

Why Your Doctor Orders Fasting Tests
The primary goal of a fasting test is to establish a “baseline” or a resting metabolic state. This gives your doctor the clearest possible picture of your body’s internal chemistry without the immediate influence of a recent meal. Think of it as measuring the quiet, steady state of your body’s engine before it starts processing any fuel (food).
This baseline is crucial for accurately diagnosing and monitoring chronic conditions like diabetes, heart disease, and kidney issues. Without fasting, elevated glucose or triglyceride levels from a recent meal could be misinterpreted as a sign of a long-term health problem, leading to misdiagnosis or unnecessary treatment. Adhering to fasting guidelines ensures the data reflects your true physiological state, which is why understanding the difference in fasting vs non-fasting blood tests is so important.
The Definitive List of Common Blood Tests That Do Not Require Fasting
For many routine screenings and health checks, you can confidently eat before your appointment. This is a significant convenience, making it easier to schedule routine blood tests no fasting is required for. Here is a detailed breakdown of the most common non-fasting blood tests.
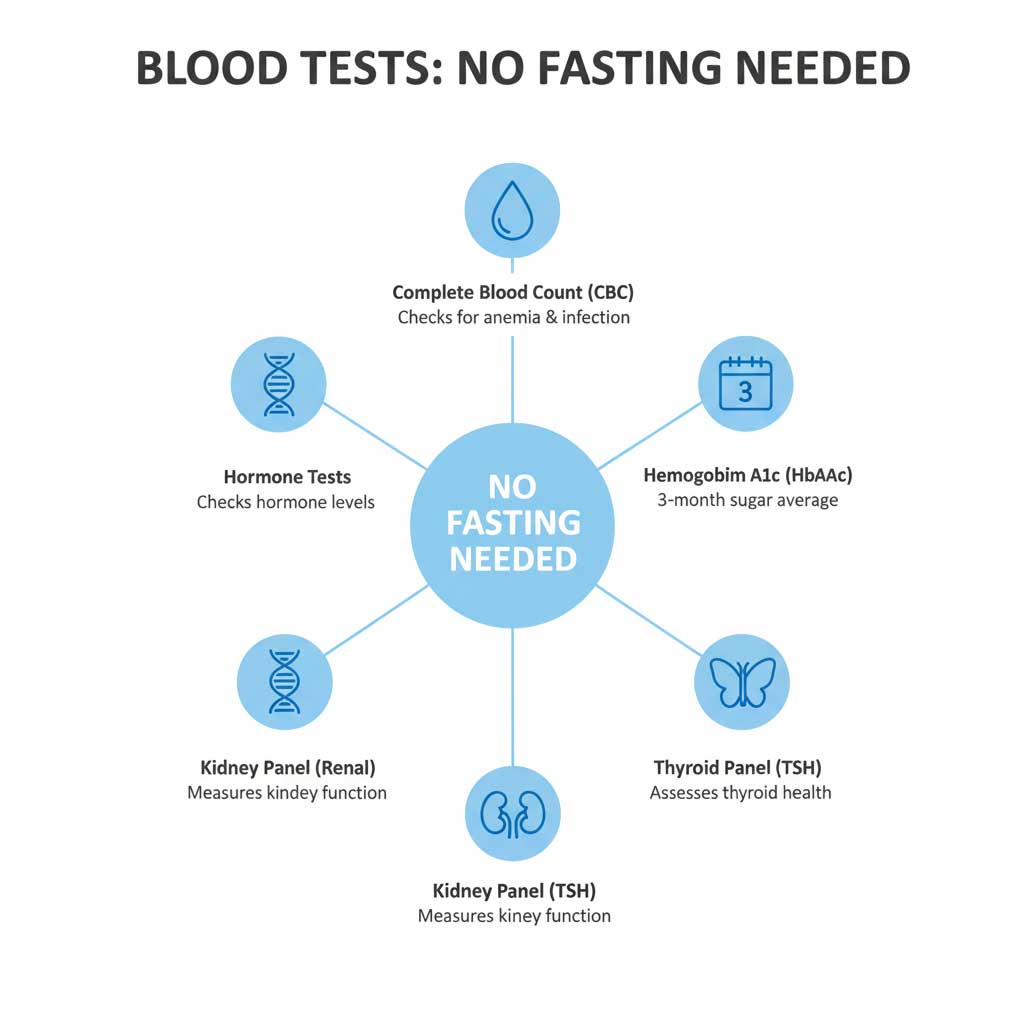
Complete Blood Count (CBC)
A Complete Blood Count is one of the most frequently ordered tests, serving as a broad indicator of your overall health. It measures the three main types of cells in your blood: red blood cells (which carry oxygen), white blood cells (which fight infection), and platelets (which help with clotting).
The key reason a complete blood count (CBC) fasting is not necessary is that the number and characteristics of these cells are not influenced by short-term food or drink intake. This test is vital for screening for a wide range of conditions, including anemia, infections, inflammation, and certain blood cancers.
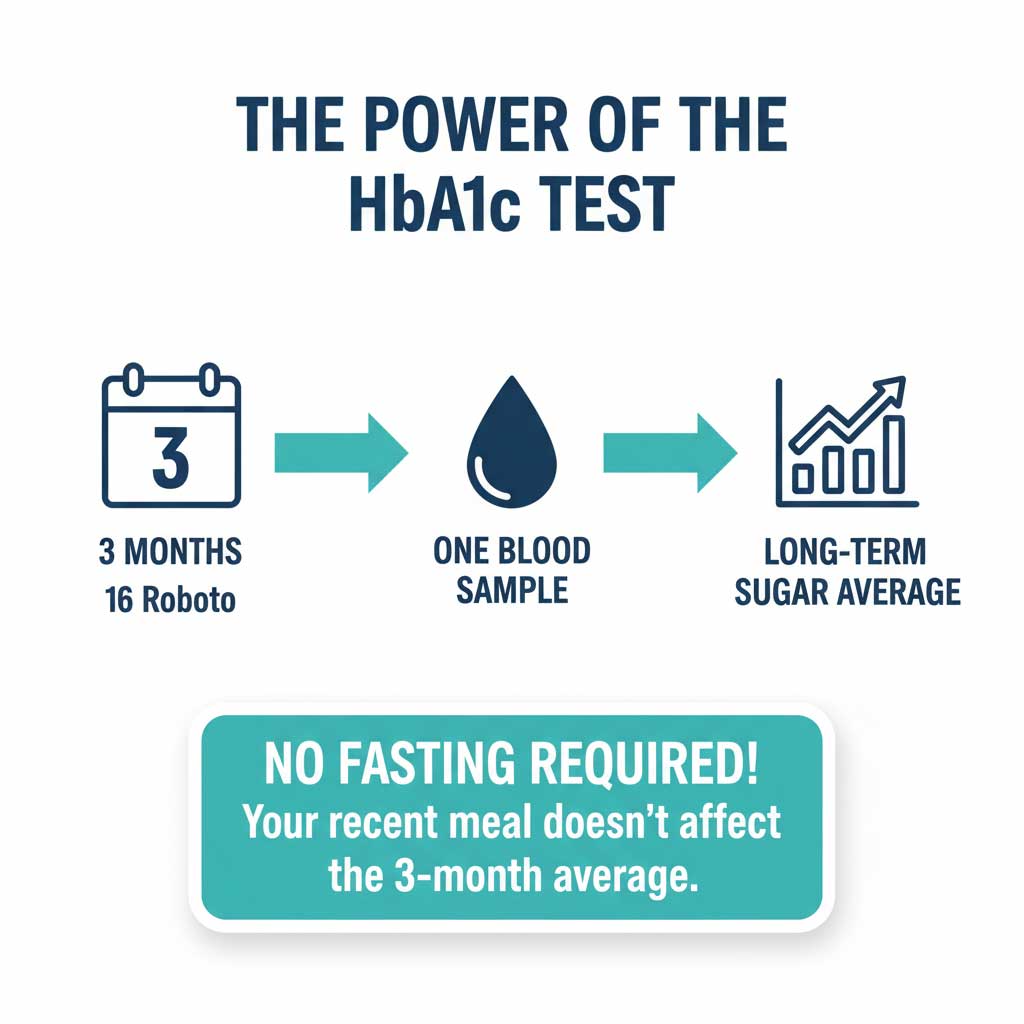
Hemoglobin A1c (HbA1c)
This is a cornerstone test for diabetes management and a prime example of a convenient non-fasting blood test. The HbA1c test provides a picture of your average blood sugar levels over the past two to three months by measuring the percentage of hemoglobin proteins in your blood that are coated with sugar.
Because it reflects a long-term average, a single meal consumed just before the test will not significantly alter the result. This makes the HbA1c test fasting rule unnecessary, offering a major advantage over fasting glucose tests for monitoring and diagnosing prediabetes and diabetes.
Thyroid Function Tests (TSH, T3, T4)
If your doctor is evaluating your thyroid health, there is generally no need to alter your eating schedule. A standard thyroid panel assesses the levels of Thyroid-Stimulating Hormone (TSH), T3, and T4 to see how well your thyroid gland is functioning.
A common question patients ask is, “do you need to fast for a TSH blood test?” The answer is almost always no. The hormonal feedback loop that controls thyroid function is not directly impacted by digestion. While some advanced research notes minor fluctuations in TSH levels throughout the day, a thyroid function test fasting is not the clinical standard for diagnosing conditions like hypothyroidism or hyperthyroidism.
Kidney Function Tests (Renal Panel)
A renal panel is used to evaluate how well your kidneys are filtering waste from your blood. These tests typically measure levels of creatinine and blood urea nitrogen (BUN), which are waste products.
These markers generally remain stable in the bloodstream regardless of a recent meal, reflecting the kidneys’ long-term filtering capacity rather than short-term dietary intake. This makes a kidney panel a standard piece of no fasting blood work.
Most Hormone and Fertility Tests
A wide array of hormone level tests can be performed without fasting. This includes tests for reproductive hormones like estrogen, progesterone, and testosterone, as well as fertility hormones such as Follicle-Stimulating Hormone (FSH) and Luteinizing Hormone (LH).
These hormones typically follow cyclical (monthly) or diurnal (daily) patterns that are not directly influenced by the food you eat. Therefore, most hormone panels are considered non-fasting blood tests, making them easier to schedule.
Latest Health Trends: The Shift Toward the Non-Fasting Cholesterol Test
One of the most significant recent updates in routine lab work involves the lipid panel, which measures cholesterol and triglycerides. For decades, this test was a classic example of a fasting requirement. However, new evidence is changing this long-standing practice.
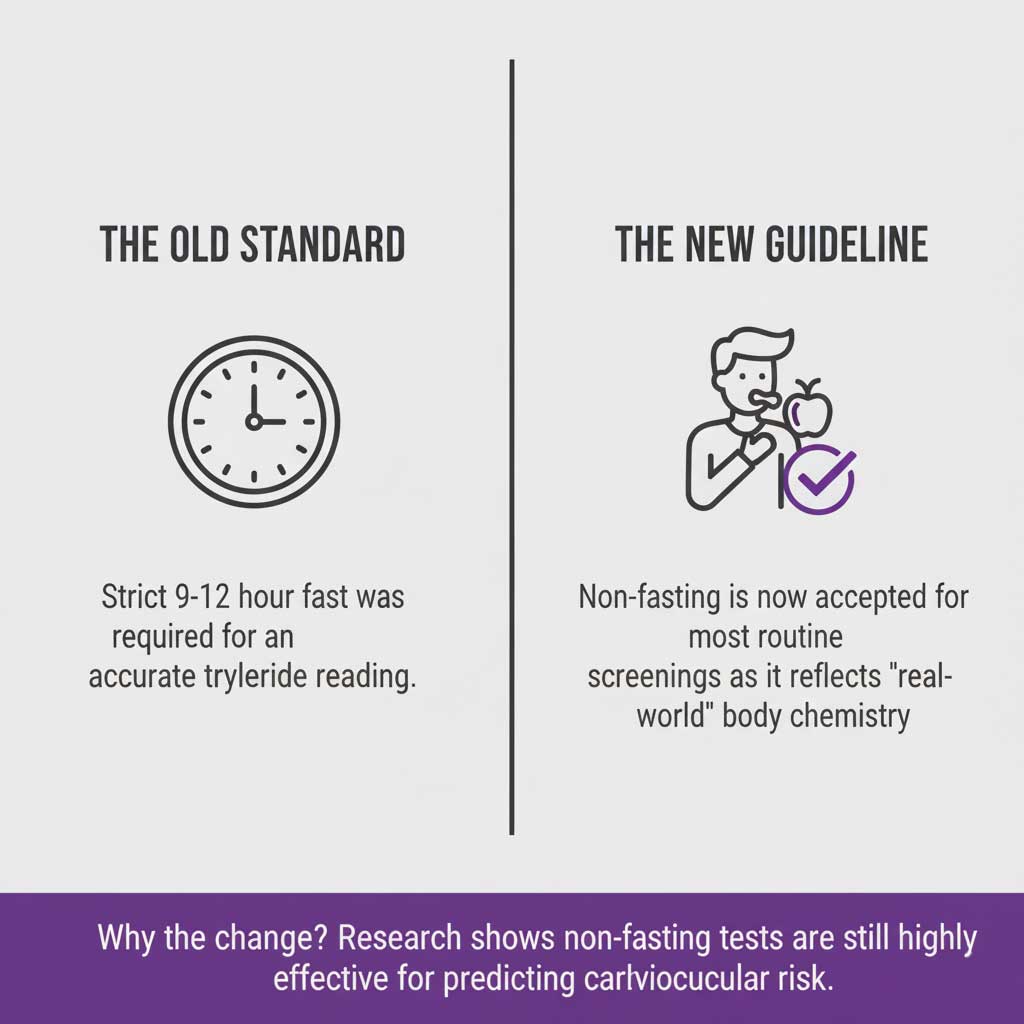
The Old Standard: Why Lipid Panels Required Fasting
The traditional lipid panel required a 9- to 12-hour fast primarily to get an accurate measurement of triglycerides, a type of fat in the blood. Triglyceride levels can rise significantly for several hours after eating a meal, particularly one high in fat or sugar. Doctors needed a baseline, fasting level to accurately assess cardiovascular risk.
New Medical Insights and Evidence
Beginning around 2016, major health organizations, including the European Atherosclerosis Society and the European Federation of Clinical Chemistry and Laboratory Medicine, released new guidelines suggesting that for most people, fasting is no longer necessary for a routine lipid panel.
Their extensive research, published in journals like the European Heart Journal, found that non-fasting cholesterol levels were just as effective, if not more so, at predicting future cardiovascular risk. The rationale is that we spend most of our day in a “non-fasting” state, so a non-fasting cholesterol test may actually provide a more realistic snapshot of our typical lipid profile.
What This Means for Patients Today
This shift means that the non-fasting cholesterol test is becoming increasingly common. It improves patient convenience and compliance, as people are more likely to get tested if they don’t have to fast.
However, it’s crucial to note that a fasting test may still be ordered in specific situations. For example, if a non-fasting cholesterol test reveals very high triglyceride levels, your doctor may order a follow-up fasting test to get a more precise baseline measurement. The best approach is always to follow the specific instructions from your healthcare provider.
Fasting vs. Non-Fasting Blood Tests at a Glance
Navigating the rules for preparing for a blood test can be simplified with a clear visual guide. This table breaks down common tests to help you understand what to expect.
| Test Category | Fasting Usually Required? | Primary Purpose | Reason for Fasting/Non-Fasting |
| Complete Blood Count (CBC) | No | General health, anemia, infection | Measures blood cells, which are not affected by food. |
| Hemoglobin A1c (HbA1c) | No | Long-term glucose monitoring | Reflects a 3-month average, unaffected by one meal. |
| Thyroid Panel (TSH, T3, T4) | No | Thyroid gland function | Hormone levels are not directly altered by digestion. |
| Kidney Panel (Creatinine, BUN) | No | Kidney filtration health | Measures stable waste products in the blood. |
| Lipid Panel (Cholesterol) | Depends (Trending toward No) | Cardiovascular risk assessment | Fasting provides a baseline triglyceride level, but a non-fasting cholesterol test is now often accepted. |
| Fasting Blood Glucose (FBG) | Yes (8+ hours) | Diabetes screening | Measures baseline blood sugar without the influence of food. |
| Metabolic Panel (BMP/CMP) | Yes (8-12 hours) | General health, organ function | Includes a glucose test, which requires fasting. |
| Iron Tests | Yes (Usually) | Anemia diagnosis, iron levels | Food intake directly affects iron absorption. |
Practical Strategies: How to Prepare for Any Blood Test
Proper preparation is key to ensuring your lab results are accurate, whether you are having non-fasting blood tests or fasting ones. Following a few simple guidelines can make the process smooth and stress-free.
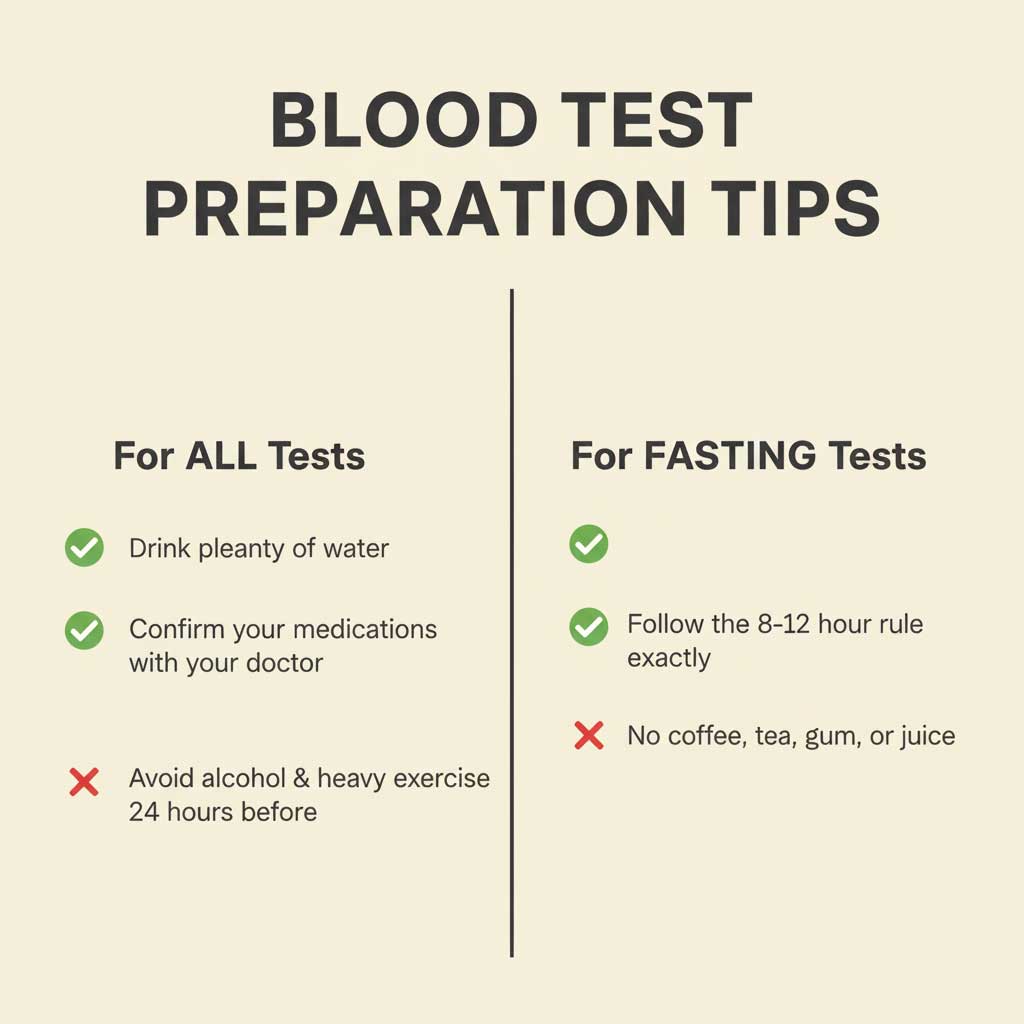
For ALL Blood Tests (Fasting or Non-Fasting)
- Hydrate Well with Water: One of the most common questions is, “can you drink water before a blood test?” The answer is a resounding yes. Staying well-hydrated makes your veins fuller and easier for the phlebotomist to find, which can make the blood draw quicker and more comfortable.
- Confirm Your Medications: Before your test, ask your doctor if you should take your usual medications as scheduled. Most are fine to take, but some, like certain supplements or diuretics, might need to be paused.
- Avoid Alcohol and Strenuous Exercise: Both alcohol consumption and intense physical activity in the 24 hours before a test can affect your results, particularly liver enzymes and hydration levels. It’s best to avoid them.
For FASTING Blood Tests
- Time It Right: The fasting window is precise. If your appointment is at 8 AM and requires an 8-hour fast, you should have nothing to eat or drink (except water) after midnight. Setting a reminder on your phone can be helpful.
- Know What to Avoid: Fasting means no food or drinks. This includes items you might not think of as a “meal,” such as chewing gum, breath mints, coffee (even black), and tea, as they can stimulate your digestive system and affect results.
Common Challenges & Misconceptions
There is a lot of misinformation surrounding blood test preparation. Let’s debunk some of the most common myths to ensure you get accurate results every time.
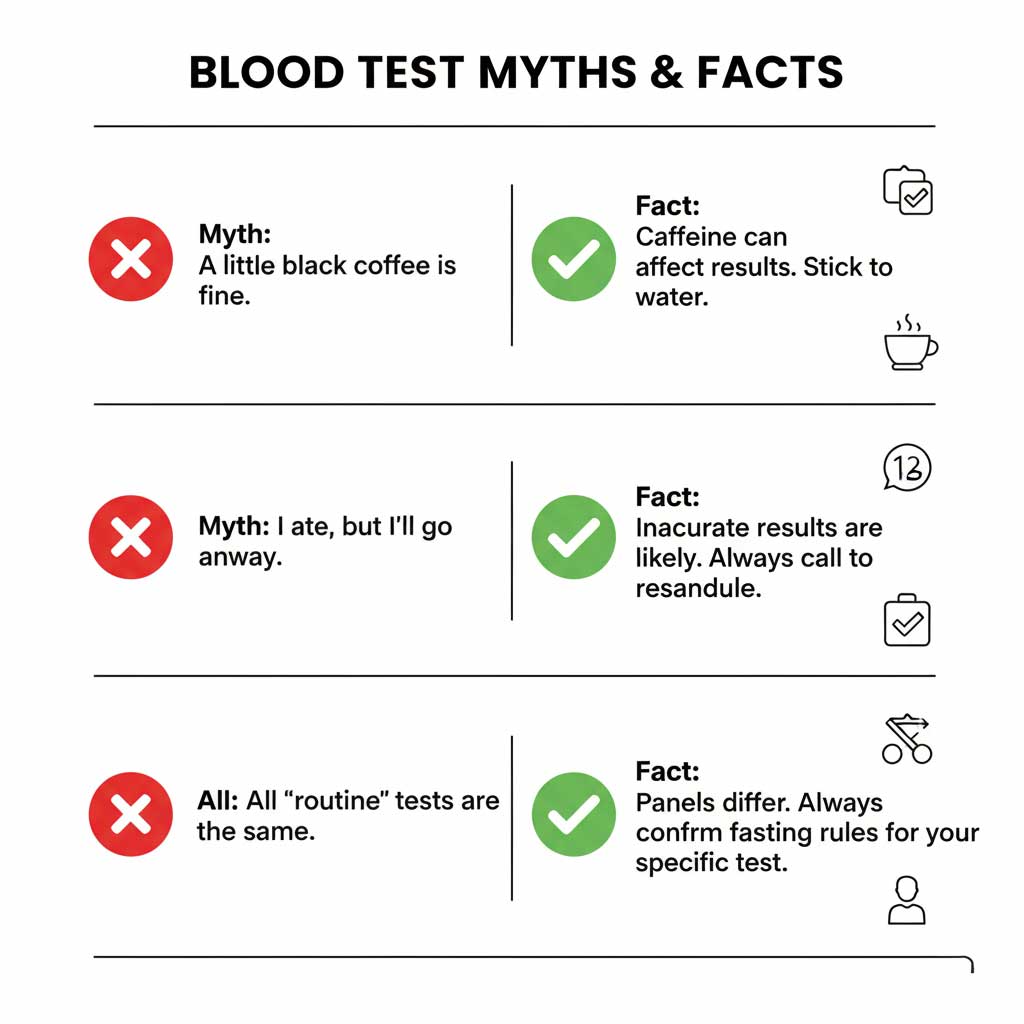
Myth 1: “A tiny bit of black coffee won’t hurt a fasting test.”
Fact: This is one of the most frequent mistakes. While black coffee has virtually no calories, caffeine is a stimulant that can affect your body’s processes. It can impact hydration levels and potentially influence glucose metabolism and blood pressure, slightly skewing the results. It’s best to stick to plain water.
Myth 2: “I accidentally ate. I should just go to the test anyway and not mention it.”
Fact: This can lead to serious diagnostic errors. It’s crucial to be honest if you’ve broken your fast. The lab needs to know what happens if I eat before a blood test that requires fasting, which is that the results will be inaccurate. Inform the phlebotomist immediately. They will likely advise you to reschedule the test to ensure your doctor receives reliable information.
Myth 3: “All routine blood tests are the same.”
Fact: The term “routine” can be misleading. A “wellness panel” ordered for an annual physical might be a list of common blood tests that do not require fasting. However, a “Comprehensive Metabolic Panel” (CMP), which is also considered routine, absolutely requires fasting because it includes a glucose test. Always clarify the exact name of your test panel and its specific requirements.
Tools, Tests, or Platforms Comparison
Understanding the differences between key diagnostic tools can help you have more informed discussions with your doctor. This is particularly important when comparing fasting vs non-fasting blood tests for conditions like diabetes.
| Health Tool / Test | Purpose | Ideal Use Case | Accuracy / Reliability | Recommended By |
| Hemoglobin A1c (HbA1c) | Long-term (3-month) average blood glucose | Diabetes diagnosis and ongoing management | High | American Diabetes Association (ADA) |
| Fasting Blood Glucose (FBG) | Measures current blood sugar at a single point in time | Initial diabetes screening, monitoring daily control | High (when fasting is done correctly) | World Health Organization (WHO) |
| Complete Blood Count (CBC) | Measures cell counts (RBC, WBC, platelets) | Routine check-up, diagnosing anemia or infection | High | Centers for Disease Control (CDC) |
| Lipid Profile (Fasting) | Checks cholesterol & triglycerides at baseline | Initial diagnosis of high cholesterol/triglycerides | High | American Heart Association (AHA) |
Ethical and Privacy Considerations in Modern Healthcare
The landscape of medical testing is expanding beyond the clinic, with a surge in at-home testing kits and digital health platforms. While these innovations offer unprecedented convenience, they also introduce important ethical and privacy considerations.
The Rise of At-Home Testing Kits
Direct-to-consumer testing kits allow you to collect a blood sample at home and mail it to a lab. These kits can test for everything from vitamin deficiencies to cholesterol. While convenient, it’s vital to ensure the company uses a certified lab (CLIA-certified in the U.S.) and to discuss the results with a healthcare professional, as context is key to understanding any health data.
Data Privacy and Your Health Information
When you use a lab, clinic, or even a health app, you are entrusting them with some of your most sensitive personal data. In the United States, the Health Insurance Portability and Accountability Act (HIPAA) provides strong protections for your health information. However, it’s wise to be cautious with third-party health apps, which may not be covered by HIPAA. Always review the privacy policy to understand how your data is stored, used, and protected.
Actionable Health Tips: Taking Control of Your Lab Work
Empower yourself with a proactive approach to your health. Use these actionable tips to ensure every blood draw experience is efficient, comfortable, and provides your doctor with the most accurate information possible.
- Always Ask Specific Questions: When you receive a lab order, ask, “Is this a fasting test? If so, for how many hours?”
- Confirm Your Medications: Proactively ask your doctor, “Should I take my morning pills before the test, or wait until after?”
- Write It Down: Keep the lab order form and any written instructions together. Make a note in your calendar with the test name and fasting requirements.
- Schedule Smart: If you need to fast, book the earliest available appointment in the morning. This minimizes the time you have to go without food and reduces discomfort.
- Communicate with the Lab: Don’t hesitate to call the lab ahead of time if you have any last-minute questions about preparing for a blood test.
Summary & Key Takeaways
In summary, navigating the world of lab work is far simpler when you know that a long list of common blood tests that do not require fasting exists. Key screenings like the Complete Blood Count (CBC), Hemoglobin A1c, thyroid panels, and kidney function tests are all examples of no fasting blood work. This knowledge provides flexibility and convenience for your routine health monitoring.
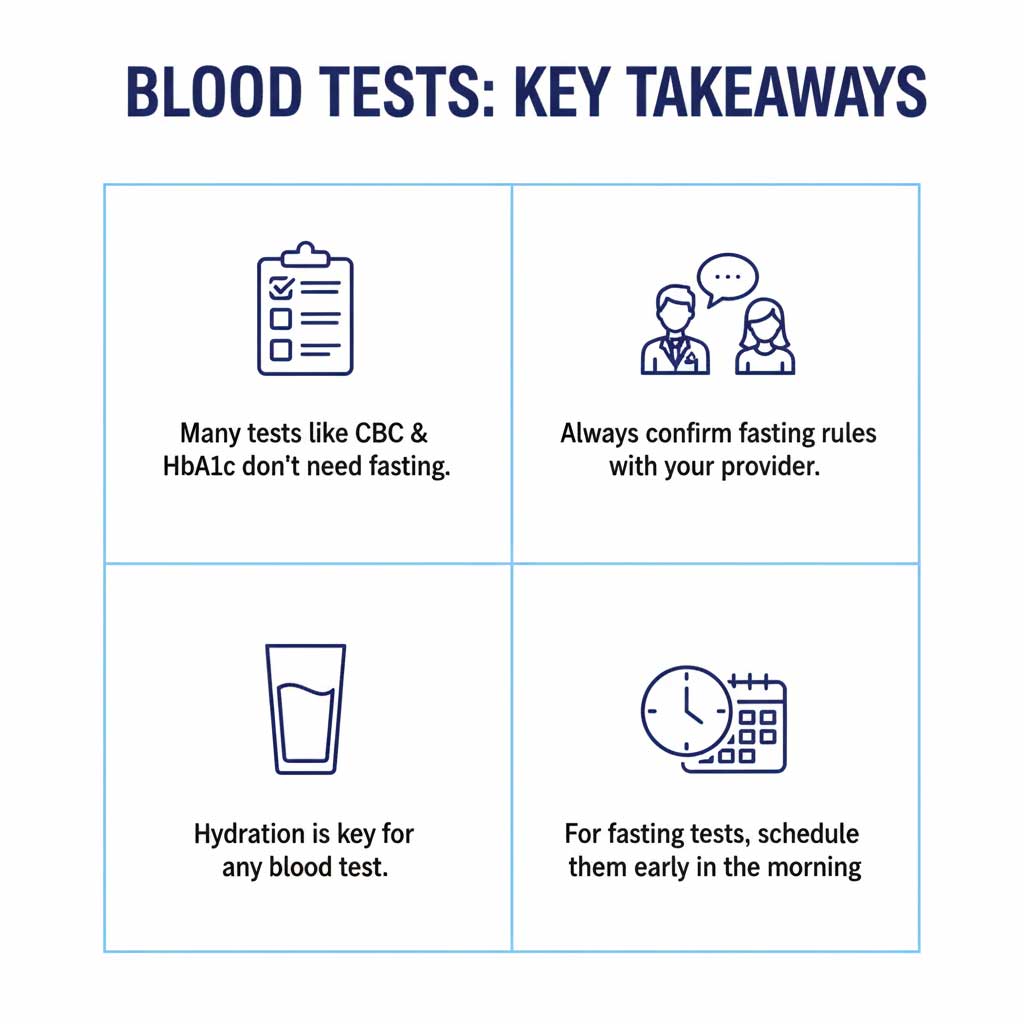
The evolving medical landscape, highlighted by the growing acceptance of the non-fasting cholesterol test, underscores a shift toward more patient-centric and practical diagnostic methods. The most critical takeaway is the importance of clear communication. By using this guide to have informed conversations with your healthcare provider, you can ensure you are always properly prepared, leading to the most accurate results and better health outcomes.
Frequently Asked Questions (FAQ)
What happens if you don’t fast for a blood test that requires it?

If you eat or drink before a test that requires fasting, substances like glucose and triglycerides will become temporarily elevated in your bloodstream. This can lead to an inaccurate result, potentially causing your doctor to misdiagnose you with a condition like prediabetes or high cholesterol. It is essential to reschedule the test if you accidentally break your fast.
Do all routine blood tests for an annual check-up require fasting?

Not necessarily. Many common routine blood tests no fasting is required for, such as a CBC or a TSH test. However, annual check-ups often include a Comprehensive Metabolic Panel (CMP) or a lipid panel, which traditionally do require fasting. Always confirm the specific tests included in your “annual check-up” panel with your doctor.
Is it better to get blood work done in the morning?

For fasting tests, scheduling an appointment for the early morning is highly recommended. This minimizes the length of time you have to go without food, as you can fast overnight while you sleep. For non-fasting blood tests, the time of day is generally not as critical, but consistency can be helpful for tests that monitor levels over time.