You sleep for nine hours, yet you wake up feeling as though you haven’t slept at all. Your limbs feel heavy, like you are moving through wet cement, and your brain struggles to retrieve simple words during conversation. This is not normal tiredness; this is a cellular energy crisis. For millions of patients, the crushing weight of fatigue and hypothyroidism remains a daily reality, even after their doctors declare their lab results “normal.”
Table of Contents
If you are reading this, you have likely sat in an exam room, desperate for answers, only to be told your TSH is within range. You may have been told your symptoms must be due to stress, aging, or depression. As a clinician focused on functional endocrinology, I hear this story every day. The disconnect between standard laboratory reference ranges and how a patient actually feels is one of the greatest failures in modern thyroid care.
True recovery requires us to look beyond the pituitary signal (TSH). We must investigate how thyroid hormone functions at the cellular level. When the cells are starved of active hormone, every system in the body slows down. This guide will walk you through the physiological mechanisms of thyroid fatigue and how to fix them.
What is Thyroid Fatigue?
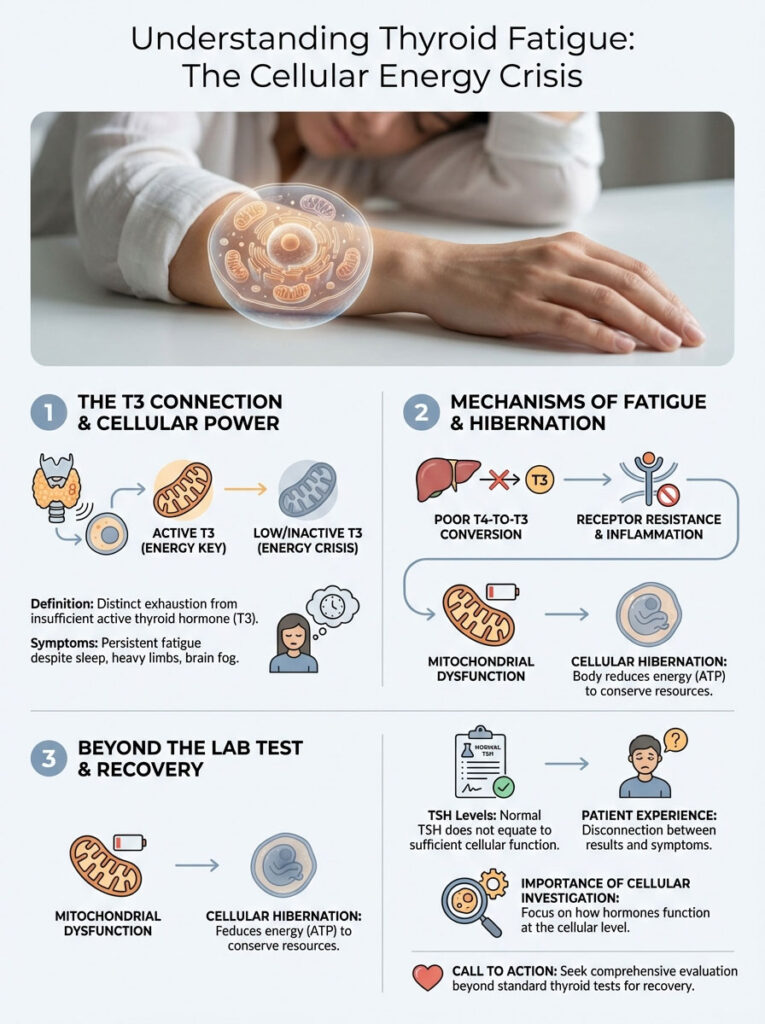
Thyroid fatigue is a distinct, pathological form of exhaustion caused by insufficient active thyroid hormone (T3) reaching the nucleus of the cell. Unlike normal tiredness, it does not resolve with sleep. It often persists despite normalized TSH levels due to poor T4-to-T3 conversion, receptor resistance, inflammation, or mitochondrial dysfunction. It is a state of cellular hibernation where the body creates less energy (ATP) to preserve resources.
Key Statistics: The Scope of the Problem
- 60% of patients with hypothyroidism continue to experience significant fatigue despite Levothyroxine therapy (Rush University Medical Center).
- 20 million Americans have some form of thyroid disease, and up to 60% are unaware of their condition (American Thyroid Association).
- 15-20% of the population carries a genetic polymorphism (DIO2) that impairs the conversion of T4 to T3.
- Hashimoto’s Thyroiditis is the cause of 90% of hypothyroidism cases in the United States.
- Ferritin levels below 30 ng/mL mimic hypothyroidism symptoms almost exactly, yet are often considered “normal” by standard labs.
- Women are 5 to 8 times more likely than men to have thyroid problems.
The Physiology of Energy: How the Thyroid Powers You
To understand why you are tired, you must understand how your body generates energy. Every cell in your body has mitochondria. These are the “power plants” of the cell. They take the food you eat and the oxygen you breathe to produce ATP (Adenosine Triphosphate). ATP is the currency of energy.
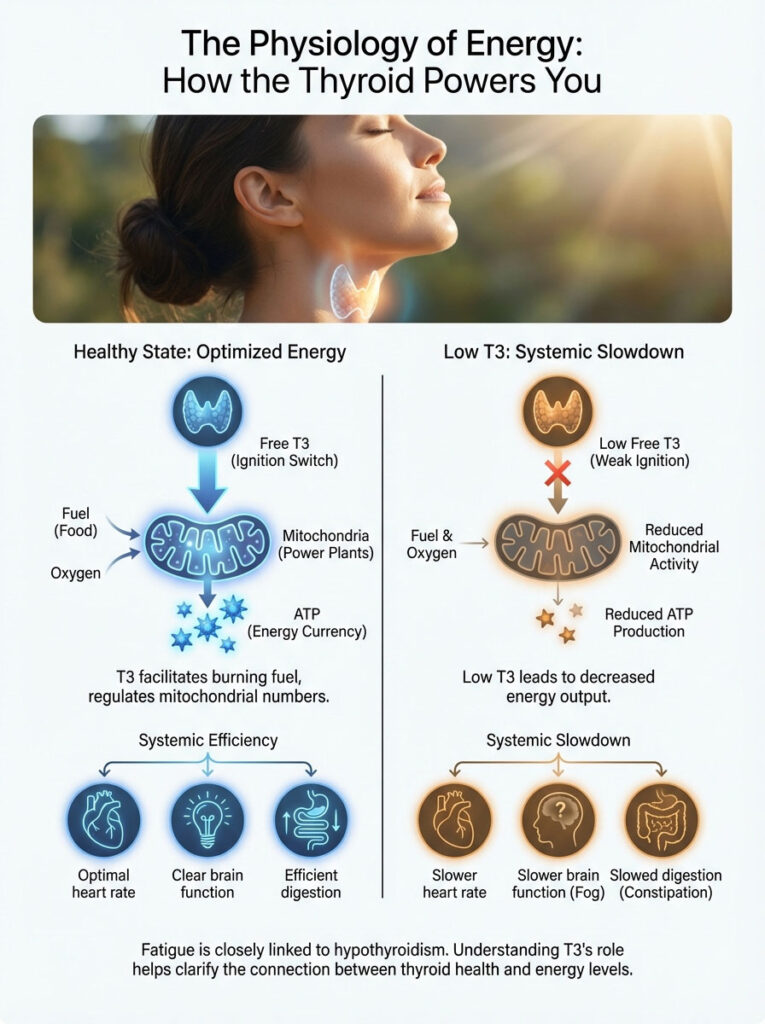
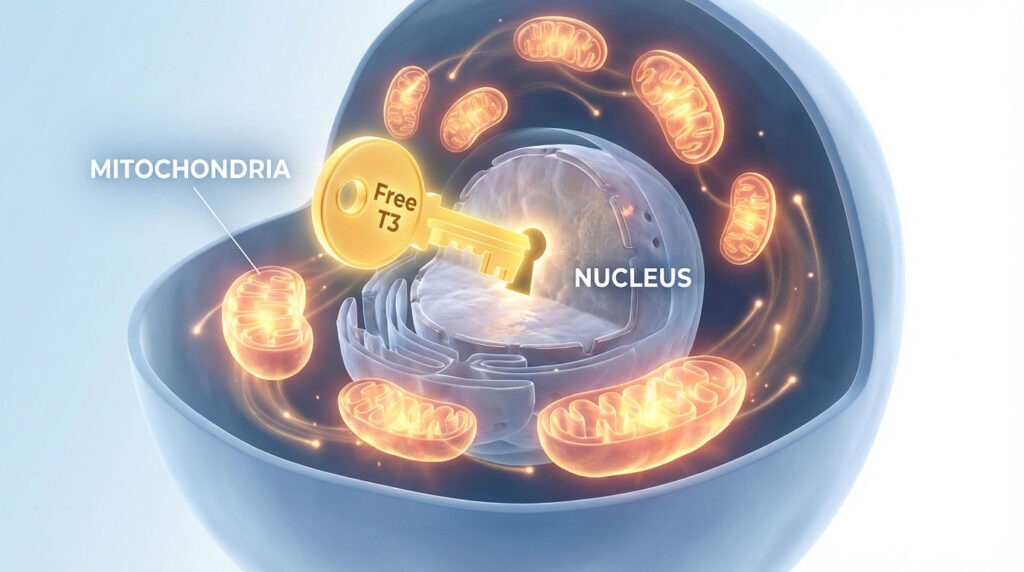
Thyroid hormone, specifically Free T3, is the ignition switch for these power plants. T3 enters the nucleus of the cell and tells the mitochondria to burn fuel. It also dictates how many mitochondria you have. When you have low T3, or when T3 cannot get into the cell, your body produces less ATP.
This results in a systemic slowdown. Your heart beats slower. Your digestion slows, leading to constipation. Your brain processes information slower. This is why fatigue and hypothyroidism are inseparable; without T3, your engine is idling in the driveway rather than driving down the highway.
The “Normal Labs” Paradox: Why Standard Testing Fails
The most frustrating phrase a thyroid patient can hear is, “Your labs look perfect.” This statement usually refers to a single marker: TSH (Thyroid Stimulating Hormone). To understand fatigue and hypothyroidism, we must first understand the limitations of TSH testing. TSH is a pituitary hormone, not a thyroid hormone. It reflects the pituitary gland’s request for more hormone, not the actual amount of active hormone available to your cells.
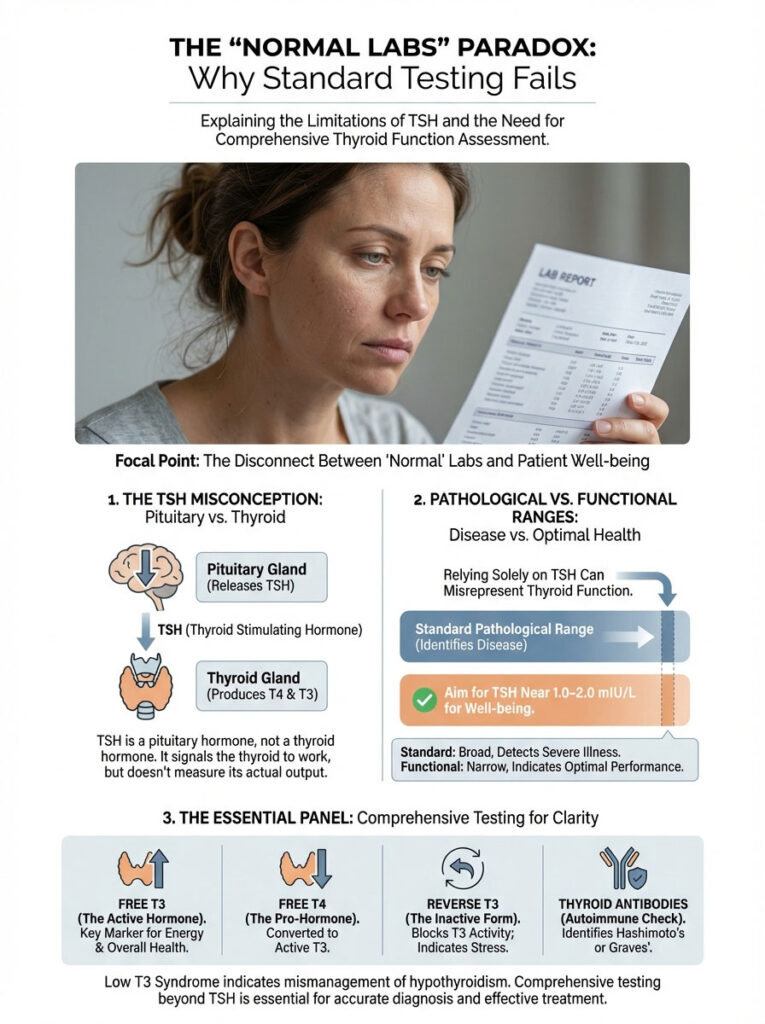
There is a massive difference between a “pathological range” and a “functional range.” Pathological ranges are averages based on the sick population visiting the lab; they are designed to identify acute disease states. Functional ranges, however, represent where the body operates optimally. A TSH of 4.0 mIU/L might be “normal” on paper, but in my practice, patients rarely feel well until their TSH is near 1.0 or 2.0 mIU/L.
Relying solely on TSH is like checking the thermostat in your hallway to determine if the bedroom is warm enough; it tells you what the system is asking for, not what the room is actually experiencing. To get the full picture, you must demand a complete panel that includes Free T3, Free T4, Reverse T3, and Thyroid Antibodies.
Comparison: Standard vs. Optimal Functional Ranges
Below is a breakdown of where your labs likely are versus where they need to be to eliminate fatigue. Understanding these numbers empowers you to advocate for better care.
| Lab Marker | Standard “Normal” Range | Optimal Functional Range | Why It Matters |
|---|---|---|---|
| TSH | 0.4 – 4.5 mIU/L | 0.5 – 2.0 mIU/L | Levels above 2.0 often correlate with brain fog and weight retention. |
| Free T3 | 2.0 – 4.4 pg/mL | 3.5 – 4.2 pg/mL | The active “gas” for the car. Low levels equal low energy. |
| Free T4 | 0.8 – 1.8 ng/dL | 1.1 – 1.5 ng/dL | Must be adequate for conversion to T3; too high can increase Reverse T3. |
| Reverse T3 | 8 – 25 ng/dL | < 15 ng/dL | Acts as a metabolic brake; high levels block energy receptors. |
| Ferritin | 15 – 150 ng/mL | 50 – 100 ng/mL | Iron is required for thyroid peroxidase activity and hormone transport. |
| TPO Antibodies | 0 – 34 IU/mL | 0 IU/mL | Presence indicates active autoimmune attack (Hashimoto’s). |
When reviewing your labs, look at the Free T3 specifically. This is the most important marker for how you feel. If your TSH is normal but your Free T3 is in the bottom 25% of the range, you will likely feel exhausted. This is a state known as “Low T3 Syndrome” or “Euthyroid Sick Syndrome,” though in a chronic setting, it is simply poor management of hypothyroidism.
The Conversion Crisis: The Deiodinase Blockade
Many patients assume that taking Levothyroxine (Synthroid) solves the problem. However, Levothyroxine is T4, a storage hormone. It is biologically inactive. It has a long half-life and floats around the blood waiting to be used. For you to feel energetic, your body must convert that T4 into T3 (triiodothyronine). This process relies on enzymes called deiodinases.
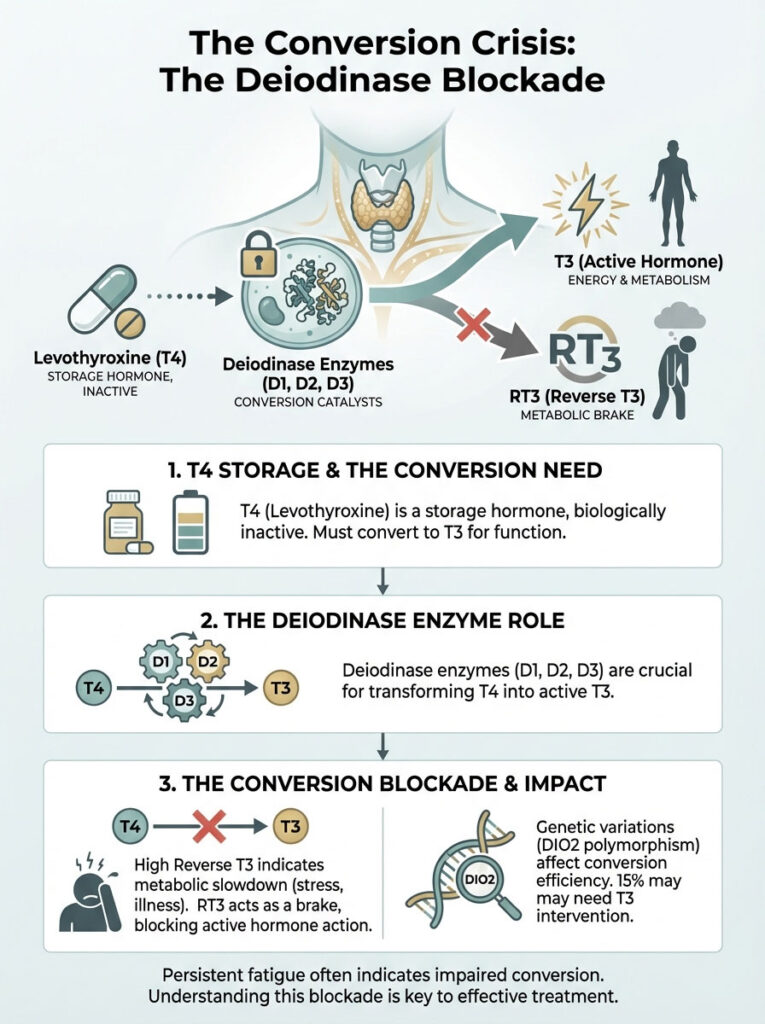
Here is the clinical reality: Fatigue and hypothyroidism often persist because this conversion process is broken. Stress, inflammation, and nutrient deficiencies can inhibit the deiodinase enzymes. Specifically, the D1 and D2 enzymes convert T4 to T3. The D3 enzyme converts T4 to Reverse T3.
Reverse T3: The Metabolic Brake
Think of thyroid receptors on your cells as parking spots. Free T3 is the car that parks there and turns on the engine (your metabolism). Reverse T3 is a car that parks in the spot but has no engine. It blocks the spot, preventing the active hormone from doing its job. When I see a patient with high Reverse T3, I know they are in a state of metabolic hibernation, regardless of how much medication they take.
Why does the body do this? It is a survival mechanism. If you are sick, starving, or under immense stress, your body wants to slow down your metabolism to save energy. It shunts T4 toward Reverse T3 to force you to rest. The problem arises when this becomes a chronic state due to modern life stressors.
The DIO2 Gene Polymorphism
We now know that genetics play a significant role. The DIO2 gene codes for the enzyme that converts T4 to T3 in the brain and other tissues. Research indicates that roughly 15% of the population has a variation in this gene that makes them poor converters. For these individuals, T4 monotherapy (Levothyroxine alone) will rarely resolve their cognitive symptoms or fatigue. They require direct T3 intervention to bypass the faulty enzyme.
Nutrient Co-Factors: The Ignored Fuel
Thyroid hormone production and conversion are chemically expensive processes. They require specific raw materials. If you are missing these co-factors, the assembly line stops. Most doctors do not test for these deficiencies, assuming a standard diet provides enough. In my experience, this is rarely true.
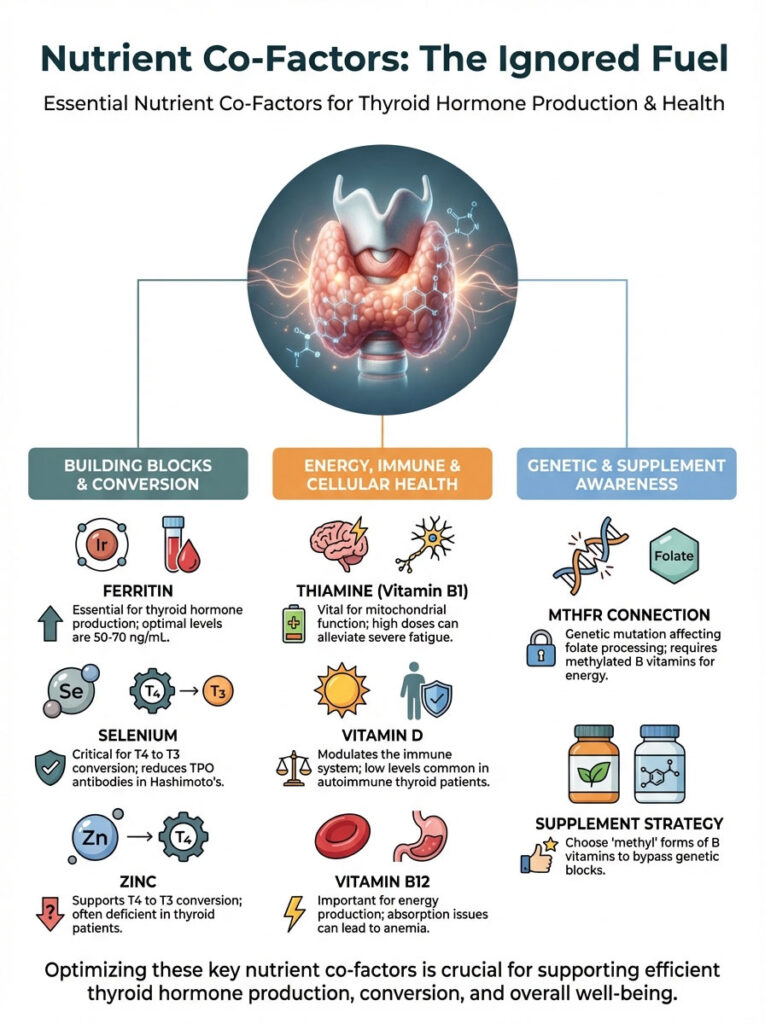
Ferritin (Iron Storage)
Iron is not just for anemia; it is the backbone of thyroid peroxidase, the enzyme that makes thyroid hormone. I frequently see women with Ferritin levels around 20 ng/mL being told they are “fine.” In reality, you need a Ferritin level of at least 50 ng/mL for hair growth and over 70 ng/mL for optimal energy. Without sufficient iron, the conversion of T4 to T3 slows down, perpetuating the cycle of fatigue and hypothyroidism.
Selenium and Zinc
The conversion of T4 to T3 happens primarily in the liver and kidneys, facilitated by selenium-dependent enzymes. A deficiency in selenium or zinc impairs this conversion. Additionally, selenium has been shown to reduce TPO antibodies in Hashimoto’s patients, calming the autoimmune attack. Brazil nuts are a famous source of selenium, but supplementation is often more consistent for therapeutic purposes.
Thiamine (Vitamin B1)
Thiamine is essential for mitochondrial function and the production of ATP. Severe fatigue that does not respond to thyroid medication often responds to Thiamine therapy. Thiamine deficiency can mimic the symptoms of hypothyroidism perfectly, including fatigue, brain fog, and low blood pressure. High-dose Thiamine (Benfotiamine or TTFD) is a common functional strategy for stubborn fatigue.
Vitamin D and B12
Vitamin D acts as a pro-hormone that modulates the immune system. Low levels are almost universal in autoimmune thyroid patients. Similarly, B12 is critical for methylation and energy production. Many hypothyroid patients have compromised stomach acid (hypochlorhydria), leading to poor absorption of B12. This results in a specific type of anemia that causes profound weakness and neurological symptoms.
Expert Insight: The MTHFR Connection
Many thyroid patients also have the MTHFR gene mutation, which affects how the body processes folate and B vitamins. If you have this mutation, taking standard folic acid can actually be harmful as it builds up in the blood. You may need methylated B vitamins (Methylfolate and Methylcobalamin) to bypass the genetic block and restore energy production. Always check your supplements to ensure they contain the “methyl” forms.
The Autoimmune Fire: Hashimoto’s and Inflammation
In the United States, the vast majority of hypothyroidism cases are caused by Hashimoto’s Thyroiditis, an autoimmune disease. This means your immune system is attacking your thyroid gland. The medical standard of care often ignores this, treating only the hormone levels while letting the autoimmune fire burn.
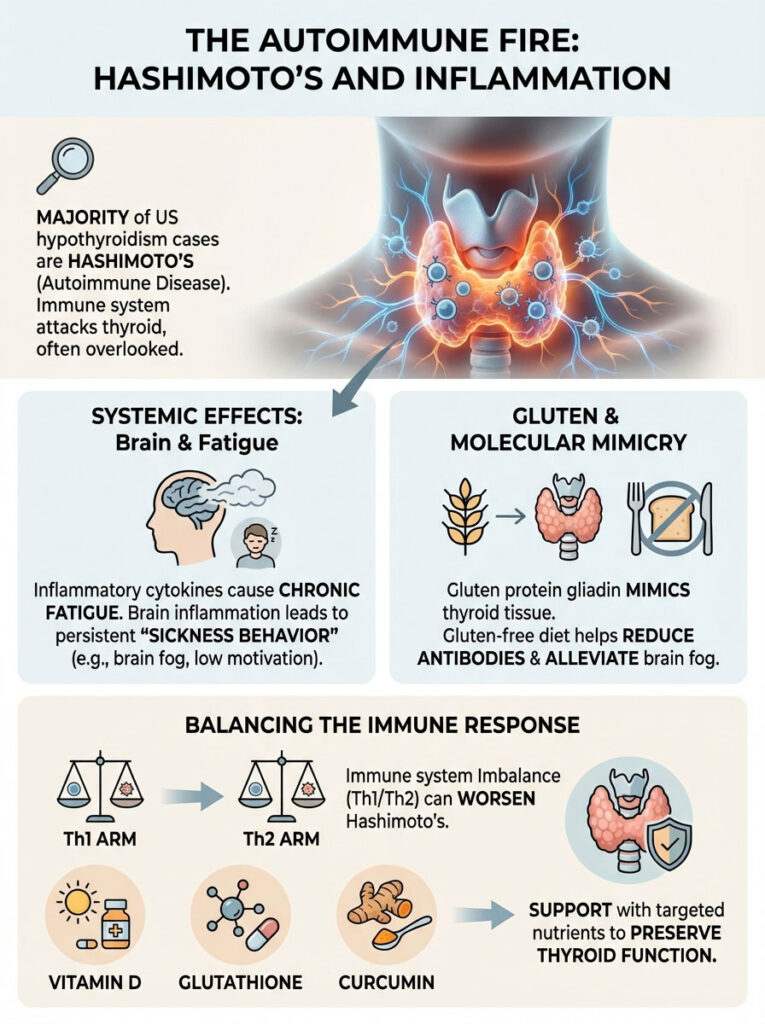
Why does this cause fatigue? When your body is under autoimmune attack, it releases inflammatory cytokines. These chemicals are messengers of the immune system. They cross the blood-brain barrier and affect the hypothalamus, leading to “sickness behavior.” This is an evolutionary mechanism designed to make you rest so the body can heal. However, in chronic autoimmunity, this signal never turns off. You feel fatigue and hypothyroidism symptoms not just because of low hormones, but because your body is fighting a constant internal war.
Gluten and Molecular Mimicry
The protein structure of gliadin (found in gluten) is strikingly similar to thyroid tissue. When you eat gluten, your immune system tags it for destruction. Because of molecular mimicry, the antibodies created to attack the gluten also attack your thyroid gland. For many of my patients, a strict gluten-free diet is the single most effective intervention for reducing antibodies and lifting the brain fog. It is not about a fad; it is about reducing the immunological burden on your system.
The Th1 vs. Th2 Balance
The immune system has two main arms: Th1 (cell-mediated immunity) and Th2 (humoral immunity). In Hashimoto’s, one of these arms is usually dominant and overactive. Factors like stress, pregnancy, and viruses can tip this balance. Balancing the immune system using immunomodulators like Vitamin D, Glutathione, and Curcumin can help dampen the attack and preserve the remaining thyroid tissue.
The Gut-Thyroid Axis: Where Energy is Lost
You cannot heal the thyroid without healing the gut. Approximately 20% of your T4 is converted to T3 by healthy bacteria in the gut (intestinal sulfatase). If you have dysbiosis—an imbalance of good and bad bacteria—this conversion drops significantly.
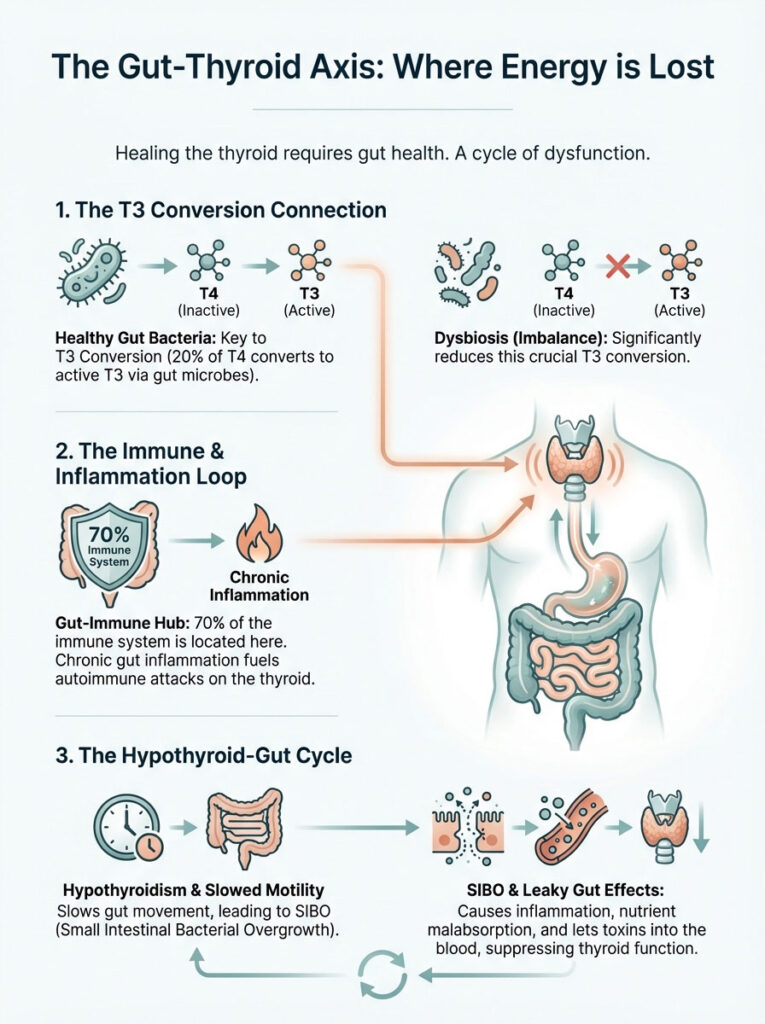
Furthermore, the gut is where 70% of your immune system resides. If your gut is inflamed, your immune system is on high alert, which fuels the autoimmune attack on the thyroid. This connection is undeniable and must be addressed for energy to return.
SIBO (Small Intestinal Bacterial Overgrowth)
There is a strong bidirectional relationship here. Hypothyroidism slows down gut motility (constipation), which allows bacteria to migrate from the colon into the small intestine, causing SIBO. SIBO then causes inflammation and malabsorption of nutrients, which worsens the thyroid condition. It is a vicious cycle. Patients with SIBO often experience bloating after meals and severe post-prandial fatigue.
Leaky Gut (Intestinal Permeability)
When the gut lining is compromised (“leaky gut”), undigested food particles and bacterial toxins (LPS) enter the bloodstream. This triggers a systemic immune response, spiking inflammation and further suppressing thyroid receptor sensitivity. Lipopolysaccharides (LPS) are toxins from bacterial cell walls that are particularly damaging to thyroid function. Healing the gut lining with L-Glutamine, Zinc Carnosine, and bone broth is often a prerequisite for thyroid recovery.
Adrenal-Thyroid Crosstalk: The HPA Axis
We often hear the term “Adrenal Fatigue,” but the correct medical terminology is HPA (Hypothalamic-Pituitary-Adrenal) Axis Dysfunction. Your adrenal glands and thyroid gland are inextricably linked. When you are under chronic stress, your adrenals pump out cortisol.

High cortisol levels have a direct suppressive effect on the thyroid:
- It suppresses the pituitary’s production of TSH, making labs look “normal” even when thyroid function is low.
- It inhibits the conversion of T4 to T3 by blocking the D2 enzyme.
- It increases the production of Reverse T3, putting the brakes on metabolism.
- It causes thyroid hormone receptor resistance on cells, meaning even if you have enough hormone, it cannot get in.
This leads to the “tired but wired” phenomenon. You are exhausted all day (fatigue and hypothyroidism) but cannot fall asleep at night because your circadian cortisol rhythm is inverted. Addressing stress through lifestyle changes and adaptogens like Ashwagandha or Rhodiola is not optional; it is a physiological requirement for thyroid recovery.
Environmental Toxins: The Chemical Assault
Our environment is filled with endocrine-disrupting chemicals that interfere with thyroid function. The thyroid gland is particularly sensitive to toxins because it is designed to uptake iodine, and many toxins mimic the structure of iodine.
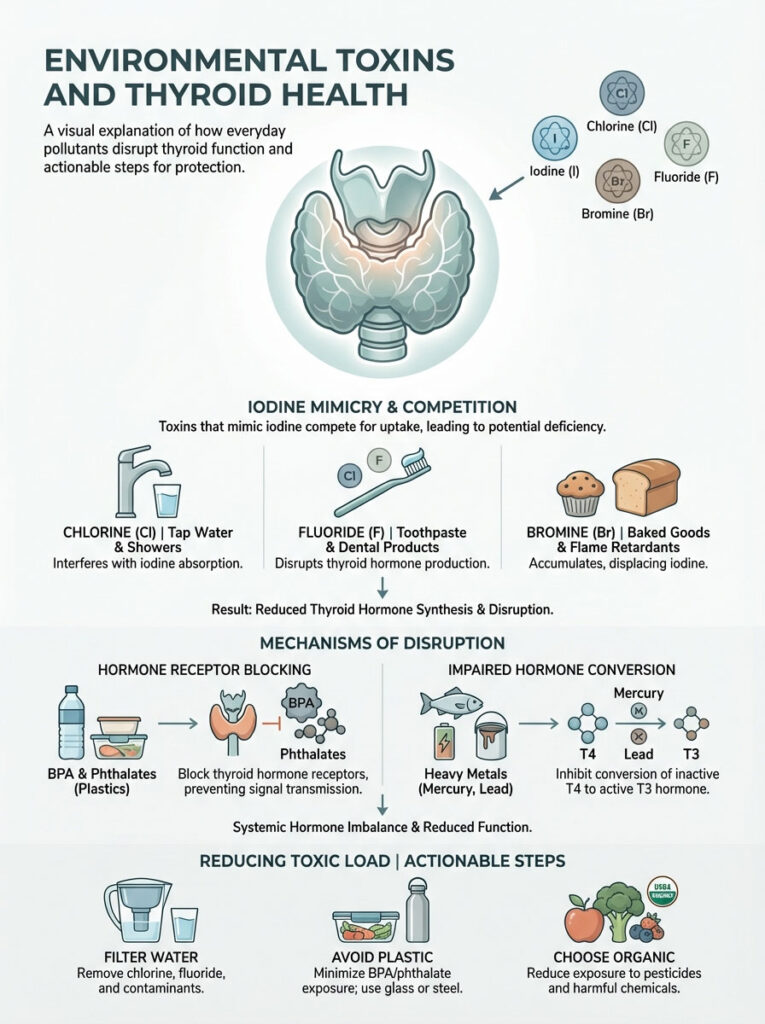
The Halogen War
Iodine is a halogen. Other halogens include Chlorine, Fluoride, and Bromine. These elements compete with iodine for absorption into the thyroid gland. We find chlorine in tap water, fluoride in toothpaste, and bromine in baked goods and flame retardants. Because these toxins are often heavier than iodine, they can displace it, leading to iodine deficiency even if you are consuming enough iodine. This prevents the formation of thyroid hormone molecules.
Plastics and Heavy Metals
Bisphenol-A (BPA) and phthalates found in plastics can bind to thyroid receptors, blocking the actual hormone from entering. Heavy metals like mercury and lead also have an affinity for the thyroid. Mercury, in particular, can interfere with the conversion of T4 to T3. Reducing your toxic load by filtering your water, avoiding plastic food containers, and choosing organic produce helps to unburden the thyroid.
Medication Management: Finding the Right Protocol
If you are optimizing your lifestyle but still struggling, your medication protocol may need adjustment. One size does not fit all. The standard approach of T4-only medication leaves a significant percentage of patients symptomatic.
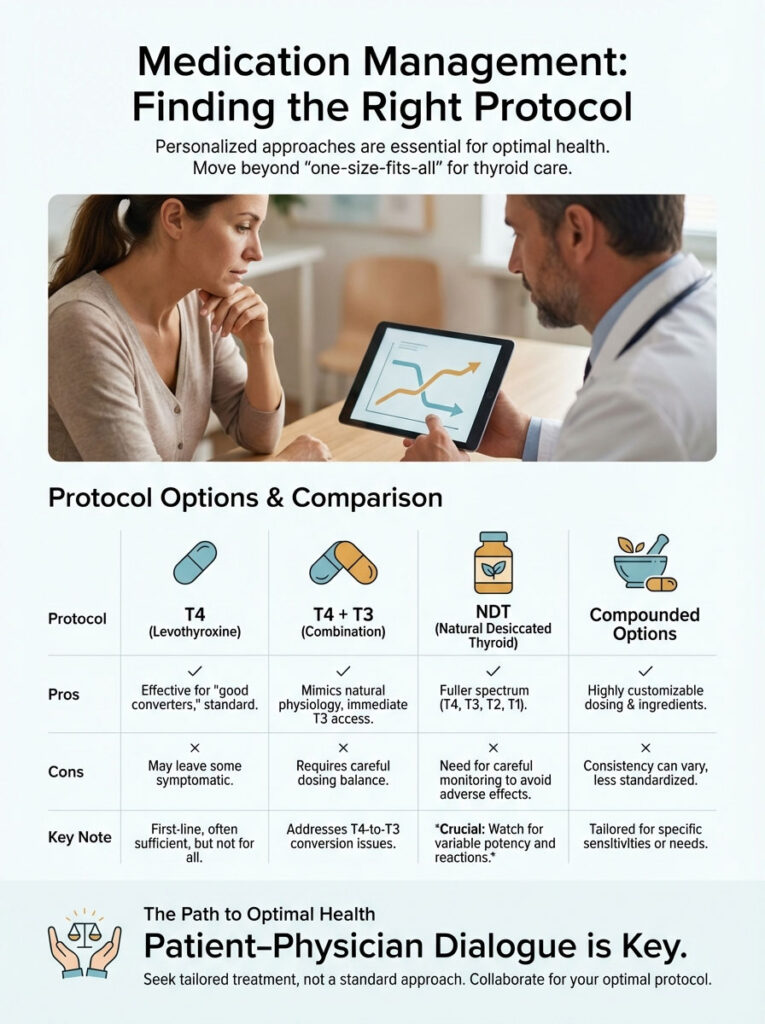
Levothyroxine (T4) Monotherapy
This is the standard of care. It works well for “good converters”—people with low stress, good gut health, and no genetic polymorphisms. However, for the complex patient, T4 alone is often insufficient to resolve fatigue. If your Free T3 remains low despite normal TSH on this medication, it is time to look at alternatives.
Combination Therapy (T4 + T3)
Adding synthetic T3 (Liothyronine/Cytomel) to a T4 regimen can be a game-changer. This ensures the body has immediate access to the active hormone, bypassing the conversion blockade. This mimics the body’s natural physiology more closely than T4 alone. The challenge is that T3 has a short half-life, so it often needs to be dosed multiple times a day to avoid energy crashes.
Natural Desiccated Thyroid (NDT)
Medications like Armour Thyroid or NP Thyroid are derived from porcine (pig) thyroid glands. They contain T4, T3, and trace amounts of T2 and T1. Many patients report feeling significantly better on NDT because it provides a full spectrum of hormones. However, the ratio of T4 to T3 in pigs is different from humans (higher in T3), so dosing requires careful monitoring to avoid palpitations or anxiety.
Thyroid Medication Comparison
Understanding the tools available to your doctor helps you ask better questions during your appointments.
| Medication Type | Common Brands | Pros | Cons |
|---|---|---|---|
| Synthetic T4 | Synthroid, Levoxyl, Tirosint | Stable potency; long half-life; standard of care. | Requires body to convert T4 to T3; often leaves patients symptomatic. |
| Synthetic T3 | Cytomel, Liothyronine | Direct energy; bypasses conversion issues. | Short half-life (rollercoaster effect); can cause palpitations if dosed wrong. |
| NDT (Porcine) | Armour, NP Thyroid | Contains T4, T3, T2, T1; feels “natural” to many. | Fixed ratio of T4:T3 may not suit everyone; potential autoimmune trigger. |
| Compounded T4/T3 | Made by compounding pharmacy | Customizable ratio; filler-free options for sensitive patients. | Expensive; insurance may not cover; consistency varies by pharmacy. |
Lifestyle & Mitochondrial Support
Ultimately, thyroid hormone works on the mitochondria. If your mitochondria are damaged by oxidative stress, they cannot produce ATP (energy), even if your thyroid levels are perfect. You must create an environment where your mitochondria can thrive.
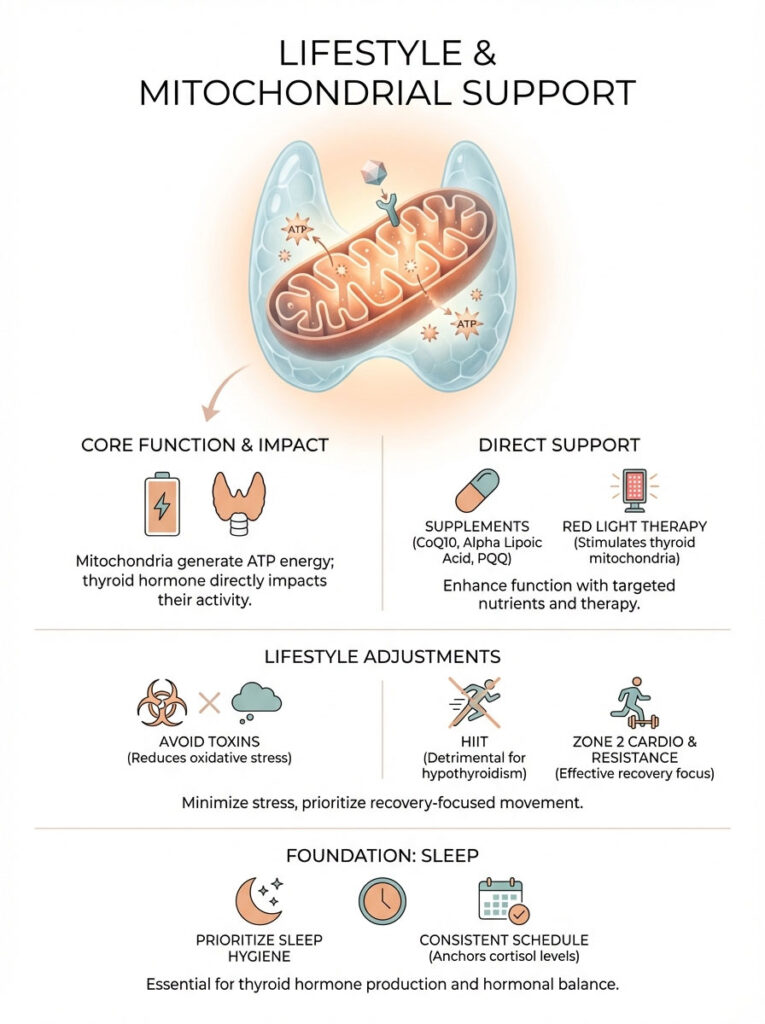
Mitochondrial Resuscitation
To support mitochondrial health, we often use supplements like CoQ10, Alpha Lipoic Acid, and PQQ. These act as spark plugs for energy production. Red light therapy (photobiomodulation) has also shown promise in stimulating mitochondrial activity in the thyroid gland itself. Furthermore, avoiding environmental toxins reduces the oxidative load on your mitochondria, allowing them to focus on energy production rather than defense.
Exercise Intolerance and Recovery
A common mistake recovering thyroid patients make is jumping into High-Intensity Interval Training (HIIT) or CrossFit. While HIIT is great for healthy individuals, it can crash a hypothyroid patient. It spikes cortisol, which we know inhibits T3. This leads to “Post-Exertional Malaise,” where a workout leaves you bedridden for two days.
Instead, focus on Zone 2 cardio (walking, light cycling where you can maintain a conversation) and resistance training. Resistance training increases the number of hormone receptors on muscle tissue, making your body more sensitive to the thyroid hormone you do have. This builds metabolic capacity without depleting your reserves.
Sleep Hygiene and Circadian Rhythm
Thyroid hormone follows a circadian rhythm. TSH naturally rises at night to stimulate thyroid production while you sleep. If your sleep is fragmented or you are exposed to blue light late at night, this signal is disrupted. Prioritizing sleep is not lazy; it is medicinal. Aim for a cool, dark room and try to wake up at the same time every day to anchor your cortisol rhythm.
Dietary Strategies for Energy
Food is information. The signals you send your body through your diet dictate your energy levels. There is no single “thyroid diet,” but there are principles that work for the majority of patients struggling with fatigue and hypothyroidism.

The Autoimmune Protocol (AIP)
For those with Hashimoto’s, the AIP diet is the gold standard for identifying triggers. It involves removing grains, legumes, nightshades, dairy, eggs, and nuts for a period of 30-90 days. This allows the immune system to calm down and the gut to heal. Once symptoms resolve, foods are reintroduced one by one to identify specific sensitivities. While restrictive, it is incredibly effective for eliminating fatigue.
Blood Sugar Balance
Hypothyroidism often comes with insulin resistance. When your blood sugar spikes and crashes, your energy does the same. Every time your blood sugar crashes, your adrenals release cortisol to bring it back up. This cortisol surge suppresses your thyroid. Eating protein and healthy fats with every meal stabilizes blood sugar and prevents these adrenal spikes.
Summary & Key Takeaways
Recovering from fatigue and hypothyroidism is rarely as simple as taking a pill. It requires a forensic investigation into your unique physiology. The “Normal Labs Paradox” is real, but it is not a life sentence. By addressing nutrient deficiencies, optimizing gut health, silencing the autoimmune response, and ensuring you are on the correct medication protocol, you can turn the lights back on.

The Bottom Line:
- Do not accept TSH as the only measure of your thyroid health; demand a full panel including Free T3 and Reverse T3.
- Check your Ferritin; if it is under 50 ng/mL, treat the iron deficiency aggressively.
- Consider if you are a poor converter of T4 to T3 and discuss combination therapy (T4 + T3) with your doctor.
- Address the autoimmune component through diet (Gluten-Free/AIP) and stress reduction to lower inflammation.
- Support your mitochondria with CoQ10, B-vitamins, and Zone 2 exercise.
You are the CEO of your own health. Use this information to advocate for the care you deserve. The path to energy is not a straight line, but with the right map, recovery is absolutely possible.
Frequently Asked Questions
Why am I still exhausted when my TSH lab results are normal?
TSH is a pituitary marker, not a direct measure of cellular energy or active hormone levels. You may still experience crushing fatigue and hypothyroidism symptoms if your Free T3 levels are low or if you have cellular resistance, even when TSH is within the standard reference range.
What are the optimal functional lab ranges for Free T3 and Free T4?
Functional medicine targets optimal levels where the body thrives rather than just avoiding acute disease. For most patients to eliminate fatigue, we aim for a TSH between 0.5–2.0 mIU/L and a Free T3 in the upper quadrant of the lab range, typically between 3.5–4.2 pg/mL.
Why isn’t Levothyroxine or Synthroid resolving my hypothyroid fatigue?
These medications provide T4, which is a storage hormone that must be converted into active T3 to generate energy. Many patients struggle with this conversion process due to inflammation, nutrient deficiencies, or genetic factors, leaving them symptomatic despite “normal” T4 levels.
How does high Reverse T3 act as a metabolic brake on energy?
Reverse T3 (rT3) is an inactive mirror image of T3 that binds to your cellular receptors and blocks active hormone from entering the cell. When rT3 is elevated—often due to chronic stress or illness—it effectively puts your metabolism into a state of hibernation to conserve resources.
What is the connection between low Ferritin and thyroid-related fatigue?
Iron is a critical co-factor for the enzyme thyroid peroxidase, which is required to synthesize thyroid hormone. Even if you are not clinically anemic, a Ferritin level below 50 ng/mL can significantly impair T4-to-T3 conversion and mimic the symptoms of hypothyroidism.
How does Hashimoto’s Thyroiditis cause fatigue beyond just low hormone levels?
Hashimoto’s is an autoimmune condition where inflammatory cytokines trigger “sickness behavior” in the brain. This internal immune war creates a state of systemic inflammation that causes profound exhaustion, which often persists even after hormone levels are replaced with medication.
Can the DIO2 gene mutation affect my response to T4-only thyroid medication?
Yes, approximately 15% of the population carries a DIO2 polymorphism that impairs the enzyme responsible for converting T4 into T3 within the brain and other tissues. These individuals often require combination therapy including direct T3 (Liothyronine) to resolve persistent brain fog and fatigue.
Why is gluten often restricted in a hypothyroidism and fatigue diet?
Due to molecular mimicry, the protein structure of gluten is strikingly similar to thyroid tissue, which can cause the immune system to mistakenly attack the gland. Removing gluten reduces the overall immunological burden and inflammatory cytokines, which often results in a significant boost in energy levels.
How does gut dysbiosis or SIBO interfere with thyroid hormone conversion?
Roughly 20% of thyroid hormone conversion occurs in the gut via the enzyme intestinal sulfatase produced by healthy bacteria. If you have an imbalance of bacteria or SIBO, this conversion process is compromised, leading to lower levels of active T3 and increased fatigue.
What is the “tired but wired” feeling in adrenal-thyroid crosstalk?
This phenomenon occurs when HPA axis dysfunction causes cortisol to spike at inappropriate times, such as late at night. High cortisol blocks thyroid receptors and increases Reverse T3, leaving you exhausted during the day but unable to achieve restorative sleep at night.
What are the benefits of Natural Desiccated Thyroid (NDT) over synthetic T4?
NDT medications like Armour or NP Thyroid contain a full spectrum of hormones, including T4, T3, T2, and T1. Many patients find this more effective for resolving fatigue because it provides the active T3 hormone directly, bypassing the need for the body to convert T4.
Why do I experience post-exertional malaise after high-intensity exercise?
High-intensity exercise can be a massive physiological stressor that spikes cortisol and further suppresses T3 production. For those with thyroid-related fatigue, switching to “Zone 2” activities like walking or light resistance training helps build metabolic capacity without depleting your hormonal reserves.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. The “functional ranges” discussed may differ from standard laboratory guidelines. Always consult a qualified healthcare professional or endocrinologist before changing your medication, starting new supplements, or making significant dietary changes.
References
- Rush University Medical Center – rush.edu – Clinical study data showing 60% of hypothyroid patients remain symptomatic on T4 monotherapy.
- American Thyroid Association (ATA) – thyroid.org – Statistics on the prevalence of thyroid disease and the high rate of undiagnosed cases in the U.S.
- Journal of Clinical Endocrinology & Metabolism – “The DIO2 Polymorphism and Thyroid Outcomes” – Research regarding the 15-20% of the population with genetic T4-to-T3 conversion impairment.
- National Institutes of Health (NIH) – nih.gov – Data on Hashimoto’s as the primary cause of hypothyroidism and the role of inflammatory cytokines in “sickness behavior.”
- Thyroid Journal – “The Role of Iron and Ferritin in Thyroid Peroxidase Activity” – Clinical evidence linking low iron stores to impaired thyroid hormone synthesis.
- World Journal of Gastroenterology – “The Gut-Thyroid Axis” – Analysis of how intestinal dysbiosis and SIBO impact thyroid hormone conversion and autoimmune triggers.
- Frontiers in Endocrinology – “Mitochondrial Dysfunction in Hypothyroidism” – Scientific review of how T3 regulates ATP production and mitochondrial biogenesis.