Why You Can’t Lose Weight
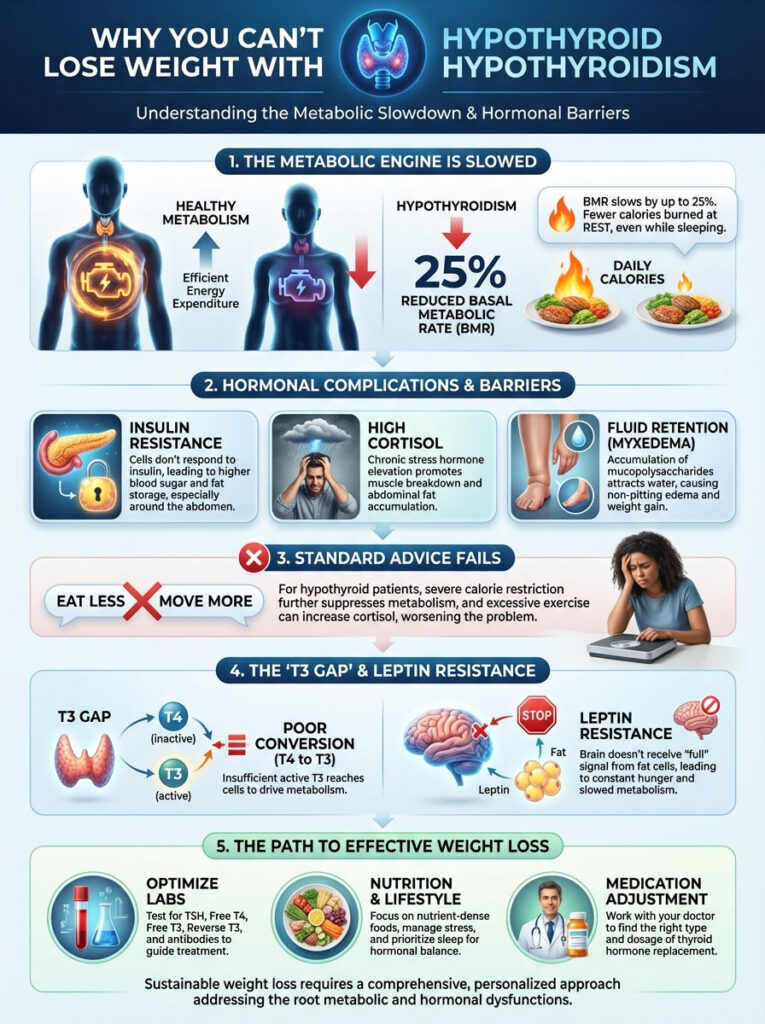
Hypothyroidism weight loss is uniquely challenging because a deficiency in active thyroid hormone (T3) lowers your Basal Metabolic Rate (BMR) by up to 25%. This means your body burns significantly fewer calories at rest than a healthy person. Furthermore, complications like insulin resistance, high cortisol, and fluid retention (myxedema) block fat oxidation. This makes standard “eat less, move more” advice ineffective and often counterproductive.
Table of Contents
You are likely reading this because you feel stuck. You track every calorie. You exercise until you are exhausted. You prioritize salads over processed food. Yet the scale refuses to budge.
Sometimes the numbers even creep higher despite your starvation efforts. In my clinical practice, I see this scenario every single day. The first thing you need to hear is this: You are not crazy. You are not lazy. You are not lying about your food intake.
Your biology is currently fighting against your efforts. The mechanism behind hypothyroidism weight loss is fundamentally different from standard weight management. The thyroid gland acts as the master gear of your metabolic engine. When that gear slows down, every cellular process in your body decelerates.
This affects everything from digestion to heat production. Standard diet advice fails hypothyroid patients because it assumes a functional metabolism. When you have an underactive thyroid, the rules of thermodynamics apply differently. Your energy expenditure is biochemically suppressed.
This guide examines the physiological barriers preventing you from losing weight. We will explore the “T3 Gap” and Leptin Resistance. We will clarify the difference between body fat and myxedema. Most importantly, we will look at how to optimize your labs, nutrition, and medication. It is time to turn the metabolic engine back on.
Key Statistics: The Thyroid-Metabolism Connection
- BMR Reduction: Untreated hypothyroidism can lower Basal Metabolic Rate by 15–25% (American Thyroid Association).
- Autoimmunity: Approximately 90% of adult hypothyroidism cases in the USA are caused by Hashimoto’s Autoimmune Thyroiditis.
- Fluid Retention: Patients can carry 5–10 lbs of non-fat fluid weight known as myxedema.
- Levothyroxine Users: Up to 15% of patients on T4-only therapy have normal TSH but low tissue levels of T3.
- Conversion Sites: 60% of T4 to T3 conversion happens in the liver; 20% occurs in the gut (microbiome).
- Muscle Tissue: Skeletal muscle burns 3x more calories at rest than fat tissue, highlighting the need for strength training.
The Physiology of a Slow Metabolism
To fix the problem, we must first understand the machinery. Your metabolism is not just a concept. It is a measurable biological process driven by hormones. When thyroid hormones are insufficient, the body enters a state of metabolic conservation.
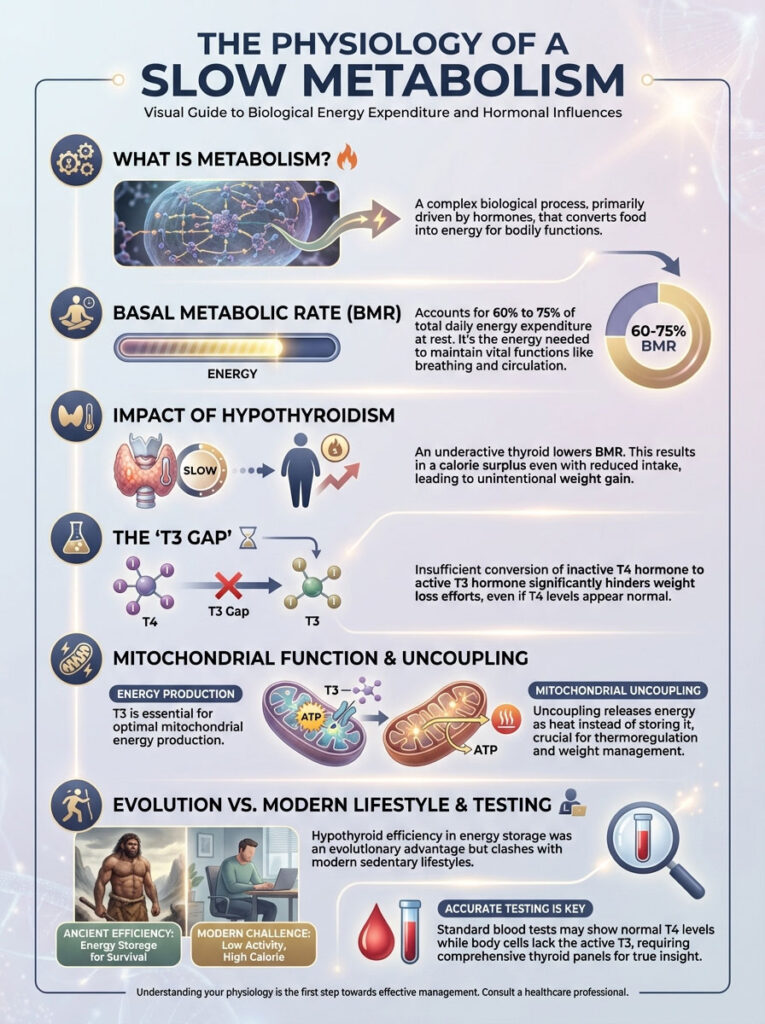
The BMR Deficit: Why Your Calorie Math is Wrong
Basal Metabolic Rate (BMR) represents the number of calories your body burns just to stay alive. This includes pumping blood, inflating lungs, and keeping your brain active. For the average person, BMR accounts for 60% to 75% of total daily energy expenditure.
In a healthy individual, the thyroid sets this “thermostat” to a comfortable temperature. However, when you have hypothyroidism, that thermostat is turned down. Clinical data suggests that BMR drops significantly when thyroid hormone levels are low.
Here is the math problem no one talks about. If your BMR should be 1,600 calories but is suppressed by 25%, you are burning only 1,200 calories. If you eat 1,400 calories, you are technically in a surplus. This is a strictly low amount of food for an adult. Yet you will gain weight.
This is why hypothyroidism weight loss feels impossible. Your “maintenance” calories are far lower than online calculators suggest. This drop occurs at the mitochondrial level. Thyroid hormone stimulates the mitochondria to produce ATP (energy) and heat. Without enough T3, mitochondria go dormant. Body temperature drops. Fat storage increases as a survival mechanism.
The “T3 Gap”: The Real Reason You Can’t Lose Weight
Most patients take Levothyroxine (Synthroid). This medication is T4. T4 is a storage hormone. It is relatively inactive. To boost metabolism, your body must convert T4 into T3. T3 is the active “gas pedal” hormone.
This conversion happens primarily in the liver and gut via deiodinase enzymes. The “T3 Gap” occurs when you have plenty of T4 (normal TSH). But your body fails to convert it into T3. You might have blood test results that look “normal” to a general practitioner.
Yet your cells are starving for active hormone. Without adequate Free T3, the signal to burn fat never reaches the cells. This conversion issue is the most common metabolic roadblock I treat. It renders T4-only medication less effective for weight loss in many patients.
Mitochondrial Uncoupling and Heat
There is another layer to this. Thyroid hormones regulate something called “mitochondrial uncoupling.” This is a process where energy is released as heat rather than stored as chemical energy. This is why hyperthyroid patients are hot and thin. They are wasting energy as heat.
Hypothyroid patients are cold and heavy. Their bodies are hyper-efficient at storing energy. You lack the T3 required to waste calories as heat. Every calorie you eat is meticulously saved. This is an evolutionary advantage for surviving a famine. It is a disaster for modern life.
Hidden Metabolic Brakes: Beyond the Thyroid
Even if your thyroid levels are optimized, other metabolic brakes can halt progress. These are secondary systems that often malfunction alongside thyroid disease. You must address the whole system.

The Reverse T3 (rT3) Blockade
Think of T3 as the gas pedal. Think of Reverse T3 (rT3) as the emergency brake. Under normal conditions, your body makes small amounts of rT3. This prevents metabolism from running too fast.
However, the body flushes the system with rT3 during periods of chronic stress. Extreme dieting triggers this. Systemic inflammation triggers this. Reverse T3 dominance creates a competitive blockade.
The rT3 molecule looks just like T3. It fits into the same receptor sites on your cells. Once rT3 parks in that spot, it does not activate the cell. It simply blocks real T3 from entering. You can have high levels of active thyroid hormone in your blood. But if rT3 is blocking the receptors, you remain hypothyroid at the cellular level.
This is often why patients feel worse after intense dieting. The calorie restriction spikes cortisol. Cortisol increases rT3. The metabolism slows down further to protect you.
Inflammation and Leptin Resistance
Most hypothyroidism is caused by Hashimoto’s. This is an inflammatory condition. When the immune system attacks the thyroid, it releases cytokines. These are inflammatory markers. Cytokines interfere with the signaling of Leptin.
Leptin is the satiety hormone produced by fat cells. It tells your brain, “We have enough fuel, burn fat.” However, chronic inflammation blunts this signal. This leads to Leptin Resistance. Your brain stops hearing the message.
Consequently, the brain thinks you are starving. It responds by increasing hunger cravings. It slows down your BMR even further. This cycle of Hashimoto’s weight gain is driven by inflammation. It is not just a lack of thyroid hormone. You cannot diet your way out of inflammation.
It’s Not Fat, It’s Myxedema
One of the most frustrating aspects of thyroid disease is the accumulation of myxedema. This is not adipose tissue (fat). It is a mucopolysaccharide gel. Specifically, it consists of glycosaminoglycans.
This gel accumulates under the skin and holds water. Myxedema vs fat is a vital distinction. Myxedema feels firm and doughy. It often appears in the face (moon face), arms, and shins.
Because this is a water-loving substance, diuretics do not work well to remove it. Calorie restriction does not burn it off because it is not energy storage. The only way to resolve myxedema is to restore optimal Free T3 levels. T3 helps the body break down the mucin deposits. This releases the trapped fluid.
Expert Insight: The “Whoosh” Effect
When patients finally achieve optimal T3 levels, they often experience a sudden drop in weight. This can be 3 to 5 pounds in a single week. This is rarely fat loss. It is the mobilization of myxedema fluid. If you notice your rings fitting looser and your face looking less puffy, your treatment is working. Do not panic if the scale stalls after this initial drop; you are now ready to burn actual fat.
Diagnostic Advocacy: Testing for Weight Loss
To achieve hypothyroidism weight loss, you must move beyond the standard TSH test. TSH (Thyroid Stimulating Hormone) is a pituitary hormone. It is not a thyroid hormone. Relying on it exclusively is dangerous.
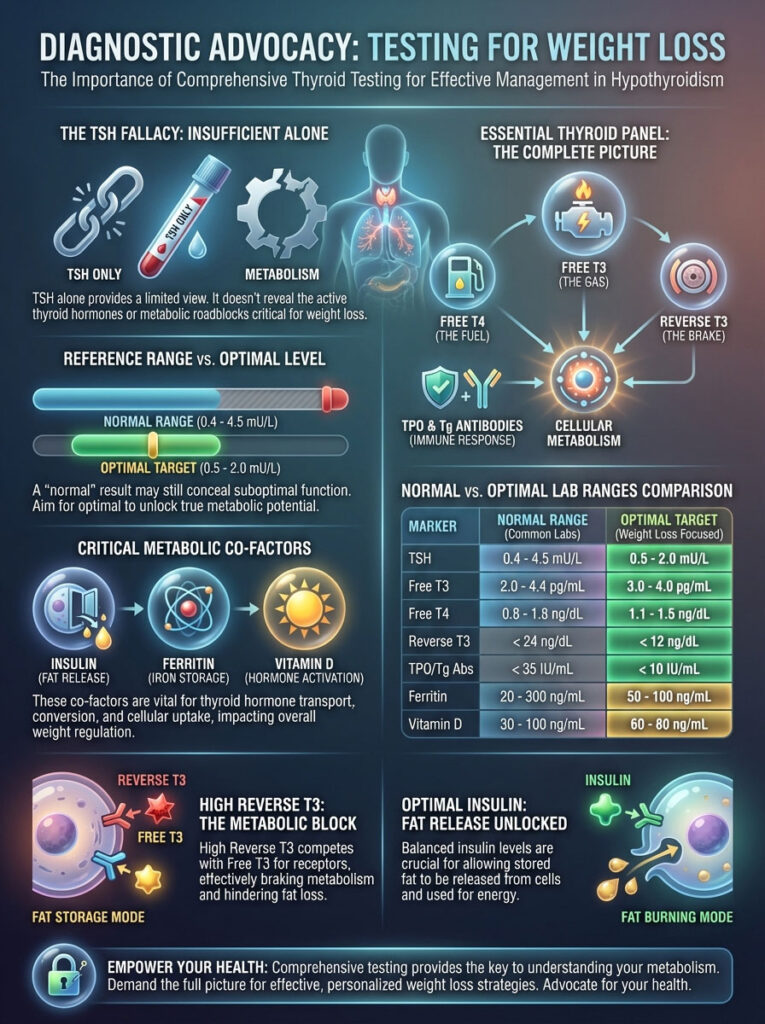
It is like trying to drive a car by looking only at the gas gauge. You are ignoring the speedometer and engine temperature. You need the full dashboard.
Why TSH is Not Enough
The standard reference range for TSH is notoriously wide. It is approximately 0.4 to 4.5 mU/L. However, the American Association of Clinical Endocrinologists has noted that a TSH above 2.5 is often associated with metabolic symptoms.
Many patients struggle to lose weight with a TSH of 3.5. They are told they are “normal.” “Normal” is a statistical average. It includes sick people. You want “optimal.” Optimal is where the body functions best.
The Essential Lab Panel for Metabolism
To get a complete picture, you need to request a full thyroid panel. This includes Free T3 (the gas) and Free T4 (the fuel). It must include Reverse T3 (the brake). You also need TPO/Tg Antibodies (the attack).
Additionally, checking metabolic co-factors is essential. Insulin, Ferritin, and Vitamin D play huge roles. If these are off, the thyroid cannot work.
Comparison Table: Normal vs. Optimal Lab Ranges
| Lab Marker | Standard “Normal” Range | Optimal Range for Weight Loss | Why It Matters |
|---|---|---|---|
| TSH | 0.4 – 4.5 mU/L | 0.5 – 2.0 mU/L | TSH > 2.5 is often linked to slower metabolic rate and difficulty losing weight. |
| Free T3 | 2.0 – 4.4 pg/mL | 3.5 – 4.3 pg/mL | Drives fat burning and energy levels. You want to be in the upper quadrant. |
| Free T4 | 0.8 – 1.8 ng/dL | 1.1 – 1.4 ng/dL | Provides the raw material for conversion without driving rT3 up. |
| Reverse T3 | 8 – 24 ng/dL | < 15 ng/dL | High rT3 blocks active hormone receptors, halting fat loss. |
| Ferritin | 15 – 150 ng/mL | > 70 ng/mL | Iron storage is required for the enzyme that converts T4 to T3. |
| Vitamin D | 30 – 100 ng/mL | 60 – 80 ng/mL | Regulates immune system function and insulin sensitivity. |
| Insulin (Fasting) | < 25 uIU/mL | < 5 uIU/mL | High insulin locks fat in cells. Optimal levels allow for fat release. |
Nutritional Strategy: Fueling the Thyroid
The underactive thyroid diet is not about cutting calories to starvation levels. That approach actually backfires. It raises Reverse T3. Instead, the goal is to reduce inflammation.

You must provide the nutrients needed for conversion. You must stabilize blood sugar. This is a targeted medical nutrition therapy.
The Anti-Inflammatory Approach
If you have Hashimoto’s, your diet must be anti-inflammatory. The most significant trigger for many patients is gluten. The molecular structure of gliadin (the protein in gluten) is strikingly similar to thyroid tissue.
This leads to a process called molecular mimicry. Eating gluten can stimulate the immune system to attack the thyroid gland. Studies suggest that a gluten-free diet can reduce TPO antibodies. It can also improve the absorption of medication.
Processed sugar is another enemy. Industrial seed oils like canola and soybean oil are also problematic. These drive systemic inflammation. By removing these, you lower the cytokine load. This helps reverse Leptin Resistance. It allows your brain to regulate appetite naturally.
The Autoimmune Protocol (AIP)
For patients with high antibodies, the Autoimmune Protocol (AIP) is often the gold standard. This is an elimination diet. It removes grains, dairy, eggs, nuts, and nightshades for a period of time.
This allows the gut lining to heal. It reduces the autoimmune attack. After 30 to 90 days, foods are slowly reintroduced. This helps identify specific triggers. Many patients find that removing dairy helps reduce myxedema swelling.
Nutrient Cofactors for Conversion
Your liver needs specific minerals to strip the iodine atom off T4 to create T3. Without these, conversion stalls. You can take all the T4 in the world, but it won’t work without these helpers.
- Selenium: This mineral is the backbone of the deiodinase enzymes. Research shows that selenium supplementation can also lower TPO antibodies. Brazil nuts are a potent source, but supplements are more consistent.
- Zinc: Essential for T3 receptor sensitivity and immune function. Zinc deficiency is common in hypothyroid patients due to poor gut absorption.
- Iron/Ferritin: Low iron is a common cause of hair loss and poor conversion in hypothyroid women. If Ferritin is under 50, metabolism suffers. You need iron to make the thyroid peroxidase enzyme work.
Managing Blood Sugar and Insulin
There is a strong correlation between insulin resistance thyroid issues and weight gain. When cells are resistant to insulin, the body stores energy as fat rather than burning it. To combat this, prioritize protein at every meal.
Aim for 30 grams of protein per meal. Protein stabilizes blood sugar. It has a higher thermic effect than carbohydrates or fats. This means you burn more calories digesting protein. Do not fear cruciferous vegetables like broccoli or kale.
Some sources claim these “goitrogens” hurt the thyroid. However, cooking them neutralizes the compounds that might theoretically slow the thyroid. Their benefits for liver detoxification far outweigh the theoretical risks. The liver needs support to convert T4 to T3.
Exercise and Lifestyle: Working With Your Physiology
Standard exercise advice can be detrimental to those with hypothyroidism weight loss goals. We need to move in a way that supports T3. We must not suppress it.

Why Chronic Cardio Makes You Fatter
Many patients sign up for marathon training. They join intense spin classes to lose weight. Then they gain weight. This is the “Cortisol-Thyroid Steal.”
Prolonged, moderate-intensity cardio raises cortisol levels. As we discussed, high cortisol increases Reverse T3 production. Essentially, by over-exercising, you are telling your body it is under stress. This causes it to hit the metabolic brakes.
Your body perceives the long run as a survival situation. It slows down the metabolism to conserve energy. This is the opposite of what you want.
The Power of Hypertrophy (Muscle Building)
The best thyroid friendly exercise is resistance training. This means lifting weights. Muscle tissue is metabolically expensive. It requires more calories to maintain than fat tissue.
By building muscle, you artificially raise your lowered BMR. Even at rest, more muscle means more T3 receptors. It means higher calorie burn. Aim for 2–3 sessions of heavy lifting per week.
Focus on compound movements. Squats, deadlifts, and presses recruit the most muscle fibers. This stimulates the greatest metabolic response without the cortisol spike of cardio.
Walking: The Underrated Fat Burner
If you must do cardio, walk. Walking is low impact. It does not spike cortisol. It improves insulin sensitivity. Aim for 8,000 to 10,000 steps a day.
This keeps the lymphatic system moving. It helps clear myxedema fluid. It does not tax the adrenals. It is the perfect complement to heavy lifting.
Sleep and Circadian Rhythm
Sleep deprivation triggers a surge in TSH. It also spikes Ghrelin (the hunger hormone). If you are sleeping less than 7 hours, your glucose metabolism degrades.
It can drop to that of a pre-diabetic within days. Prioritizing sleep is arguably as effective as diet for hormonal regulation. You must sleep to heal the HPA axis.
Medical Interventions: When Diet Isn’t Enough
Sometimes, lifestyle changes alone cannot bridge the gap. If you have a genetic polymorphism (DIO2 gene) that impairs conversion, you need help. If your gland has atrophied significantly, you need precise medical intervention.
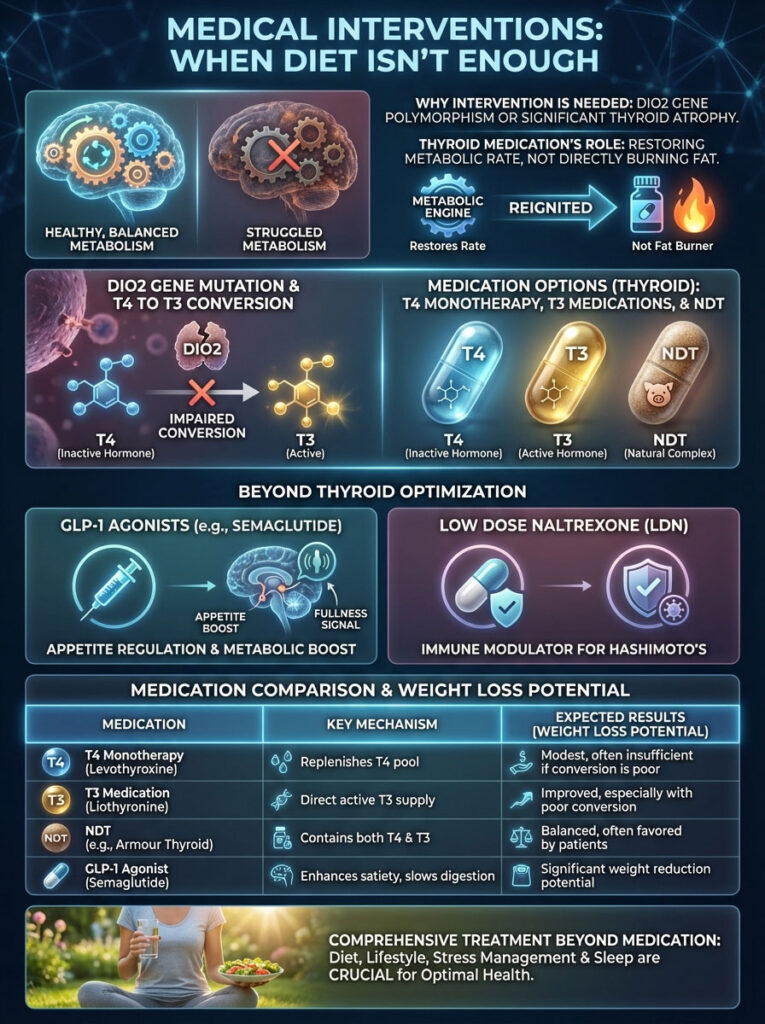
Optimizing Thyroid Medication
Thyroid medication weight loss is often a misunderstood concept. Medication does not burn fat directly. It restores the metabolic rate to normal so you can burn fat.
For many, T4 monotherapy (Levothyroxine) is insufficient. Adding a T3 medication (Liothyronine/Cytomel) can be game-changing. Switching to Natural Desiccated Thyroid (NDT) like Armour or NP Thyroid is another option.
These options provide active T3 directly. They bypass the liver conversion issue. This is crucial for patients with liver congestion or genetic conversion issues.
The DIO2 Gene Mutation
Some patients have a variation in the DIO2 gene. This gene codes for the deiodinase enzyme that converts T4 to T3 inside the cells. If you have this mutation, you are genetically poor at converting T4.
Standard blood tests might look normal because the T3 in the blood is fine. But the T3 inside the brain and muscle cells is low. These patients typically respond best to combination T4/T3 therapy.
GLP-1 Agonists and Hypothyroidism
In recent years, GLP-1 agonists like Semaglutide have become prominent. For hypothyroid patients with severe insulin resistance, these can be useful tools. They work by mimicking satiety hormones.
They regulate blood sugar and slow gastric emptying. However, they should always be used in conjunction with thyroid optimization. They are not a replacement for fixing the underlying hormonal deficiency. If you stop the drug without fixing the thyroid, the weight returns.
Low Dose Naltrexone (LDN)
LDN is an immune modulator. It is often used for Hashimoto’s patients. It helps regulate the immune system. It can lower TPO antibodies.
By reducing the autoimmune attack, inflammation drops. This can improve thyroid function and reduce Leptin resistance. It is not a weight loss drug, but it removes a major barrier to weight loss.
Comparison Table: Thyroid Medications & Weight Loss Potential
| Medication Type | Common Names | Mechanism | Weight Loss Potential |
|---|---|---|---|
| T4 Monotherapy | Levothyroxine, Synthroid | Provides storage hormone only. Relies on body to convert. | Low to Moderate (Works only if liver conversion is efficient). |
| T3 Monotherapy | Cytomel, Liothyronine | Provides active hormone directly. | High (Directly stimulates metabolism, but has a short half-life). |
| NDT (Natural Desiccated) | Armour, NP Thyroid | Contains T4, T3, T2, and T1. | Moderate to High (Mimics natural gland output). |
| Compounded T4/T3 | Custom Mix | Bio-identical, sustained release T3. | High (Customizable to patient’s unique T3 gap). |
The Role of Gut Health in Metabolism
We cannot discuss thyroid health without discussing the gut. The gut and thyroid are intimately connected. This is often called the “Gut-Thyroid Axis.”
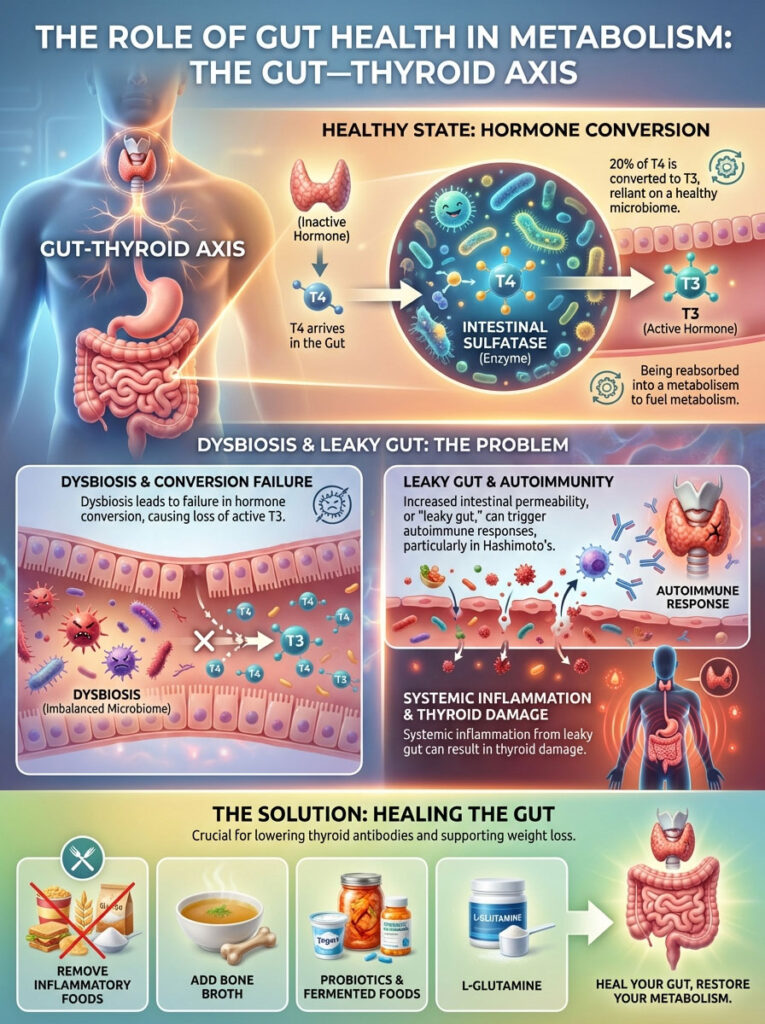
The Microbiome’s Role in Conversion
Did you know that 20% of your T4 is converted to T3 in the gut? This requires a healthy microbiome. Beneficial bacteria produce an enzyme called intestinal sulfatase.
This enzyme is required to activate thyroid hormone. If you have dysbiosis (an imbalance of bacteria), this conversion fails. You lose 20% of your active hormone right there.
Leaky Gut and Autoimmunity
There is a saying in functional medicine: “All disease begins in the gut.” This is especially true for Hashimoto’s. Increased intestinal permeability, or “leaky gut,” allows food particles into the bloodstream.
The immune system tags these particles as invaders. This creates systemic inflammation. This inflammation triggers the thyroid attack. Healing the gut is often the first step in lowering antibodies.
Steps to Heal the Gut
To support hypothyroidism weight loss, you must repair the gut. This involves removing inflammatory foods (gluten, dairy). It involves adding bone broth for collagen.
It involves taking probiotics to restore healthy bacteria. Fermented foods like sauerkraut are excellent. L-Glutamine is an amino acid that helps seal the gut lining. A healthy gut ensures that your medication is actually absorbed.
Stress Management: The Missing Link
You can have the perfect diet. You can have the perfect medication. But if you are chronically stressed, you will not lose weight. The HPA axis (Hypothalamus-Pituitary-Adrenal) communicates directly with the HPT axis (Hypothalamus-Pituitary-Thyroid).
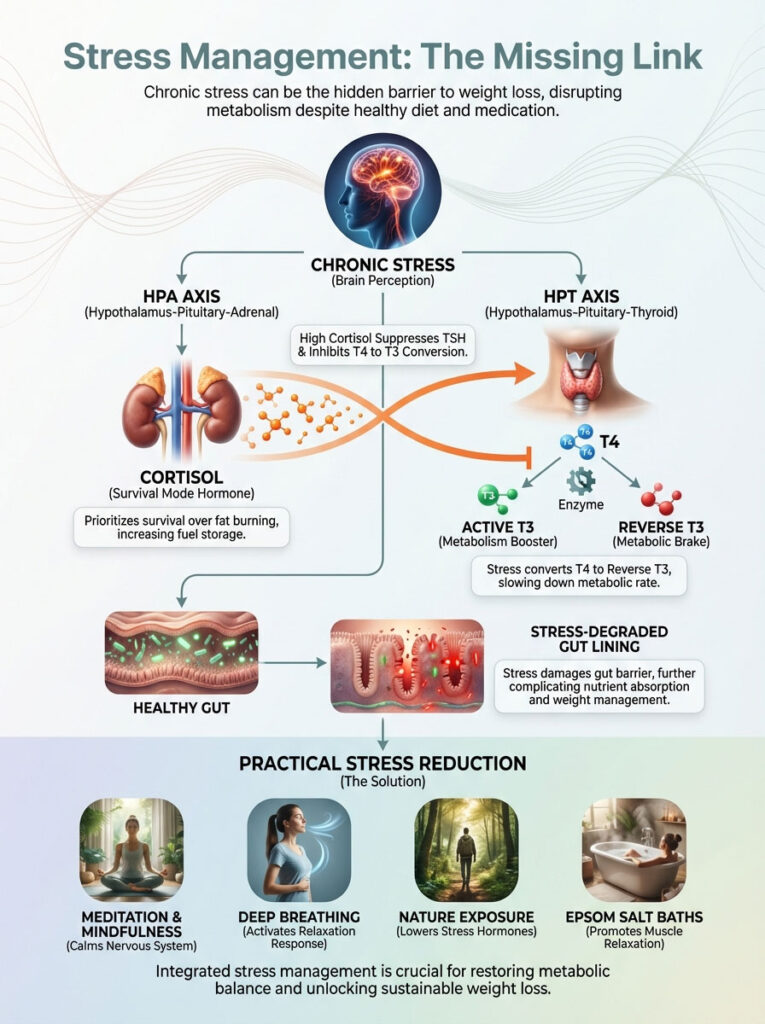
The Cortisol Steal Explained
When you are stressed, your body prioritizes survival over metabolism. It produces cortisol. Cortisol suppresses TSH. It inhibits the conversion of T4 to T3.
It increases the conversion of T4 to Reverse T3. It also degrades the gut lining. This is a quadruple whammy for your metabolism. You cannot burn fat when your body thinks it is being chased by a tiger.
Practical Stress Reduction
Meditation is not just for monks. It is a physiological intervention. Ten minutes of deep breathing can lower cortisol. Epsom salt baths provide magnesium and relaxation.
Spending time in nature lowers stress hormones. You must actively manage your stress. It is as important as taking your pill. If you are in a high-stress job or relationship, your weight loss will be slower. You must account for this.
Summary & Key Takeaways
Achieving hypothyroidism weight loss requires a shift in perspective. You are not fighting fat. You are fighting a slowed metabolic engine. You are fighting inflammation and hormonal imbalances.

The “calories in, calories out” model is broken for you until you fix the machinery. You cannot shame yourself into a faster metabolism. You must treat the physiology.
To succeed, you must become the CEO of your own health. Demand comprehensive lab testing that looks at Free T3 and Reverse T3. Adopt a nutrient-dense, anti-inflammatory diet that removes triggers like gluten.
Shift your exercise focus from chronic cardio to muscle building. Prioritize sleep and stress management. And finally, work with a practitioner who understands that “normal” lab ranges are not optimal.
By addressing the root causes—the T3 gap, insulin resistance, and inflammation—you can reignite your metabolism. You can reclaim your health. The weight loss will follow the health gain.
Frequently Asked Questions
Why does hypothyroidism lower my basal metabolic rate so drastically?
Hypothyroidism causes a deficiency in active T3 hormone, which acts as the primary metabolic thermostat for your cells. This deficiency can suppress your Basal Metabolic Rate (BMR) by 15% to 25%, meaning your body burns significantly fewer calories at rest for basic functions like breathing and circulation than a healthy individual.
Why am I unable to lose weight even though my TSH is normal on Levothyroxine?
Many patients experience a “T3 Gap” where their TSH looks normal on T4-only medication, but their body fails to convert that T4 into active T3. Without sufficient Free T3 to signal fat oxidation at the cellular level, your metabolism remains biochemically suppressed despite having lab results that appear “normal” to a general practitioner.
How can I tell the difference between actual body fat and hypothyroid myxedema?
Myxedema is a non-fat fluid retention caused by the accumulation of mucopolysaccharides under the skin, often resulting in a “doughy” or puffy appearance in the face and limbs. Unlike adipose tissue, myxedema does not respond to calorie restriction and only resolves once Free T3 levels are optimized to help the body break down and release these trapped fluids.
How does high Reverse T3 act as a metabolic brake during weight loss efforts?
Reverse T3 (rT3) is an inactive hormone that competes for the same cellular receptors as active T3. When rT3 levels are elevated—often due to chronic stress, inflammation, or extreme dieting—it effectively blocks active T3 from entering the cell, halting your metabolic engine regardless of how much thyroid hormone is circulating in your bloodstream.
Is a gluten-free diet truly necessary for Hashimoto’s weight loss?
For many Hashimoto’s patients, gluten triggers molecular mimicry where the immune system confuses thyroid tissue with gluten proteins, worsening the autoimmune attack. Removing gluten can lower TPO antibodies and reduce systemic inflammation, which helps resolve leptin resistance and allows the brain to properly regulate appetite and energy expenditure.
Why does intense cardio often cause hypothyroid patients to gain weight?
Prolonged, moderate-intensity cardio can spike cortisol levels, which signals the body to increase Reverse T3 production as a protective measure. This “metabolic braking” effect causes the body to conserve energy and store fat more efficiently, making resistance training a much safer and more effective option for thyroid patients.
What are the optimal thyroid lab ranges for successful weight loss?
To achieve weight loss, you should aim for “optimal” rather than just “normal” lab ranges, typically targeting a TSH between 0.5–2.0 mU/L and a Free T3 in the upper 25% of the reference range. Additionally, keeping Reverse T3 below 15 ng/dL is essential to ensure that thyroid hormone receptors are not being blocked.
How does insulin resistance impact weight gain in hypothyroid patients?
Hypothyroidism and insulin resistance frequently co-exist, creating a hormonal environment where high insulin levels “lock” energy into fat cells. When cells are resistant to insulin, the body struggles to access stored fat for fuel, making it necessary to address blood sugar stability alongside thyroid optimization to see results on the scale.
Which nutrients are essential for converting T4 into the active T3 hormone?
The conversion of T4 to T3 requires specific deiodinase enzymes that are dependent on selenium, zinc, and iron. If your ferritin levels are below 70 ng/mL or you have a selenium deficiency, your liver and gut cannot efficiently produce the active T3 needed to maintain a healthy metabolic rate.
Can adding T3 medication like Cytomel help with stubborn weight loss?
For patients with genetic conversion issues or liver congestion, adding a T3 medication (Liothyronine) or switching to Natural Desiccated Thyroid (NDT) can be game-changing. These options provide the active hormone directly to the cells, bypassing the conversion roadblocks that often make T4-only therapy ineffective for weight management.
How does gut health influence thyroid hormone levels and metabolism?
Approximately 20% of T4 to T3 conversion occurs in the gut via the action of beneficial bacteria and intestinal sulfatase enzymes. Dysbiosis or “leaky gut” can impair this conversion process and trigger the systemic inflammation that drives Hashimoto’s, making gut repair a foundational step in restoring metabolic function.
Why is stress management considered a “medical” requirement for thyroid weight loss?
Chronic stress activates the HPA axis, leading to sustained high cortisol which directly inhibits the production of TSH and the conversion of T4 to T3. Without managing stress, the body remains in a “survival mode” that prioritizes energy storage over fat burning, regardless of how strictly you follow a diet.
Disclaimer
This article is for informational purposes only and does not constitute medical advice. Hypothyroidism is a complex medical condition that requires professional diagnosis and management. Always consult a qualified healthcare professional or endocrinologist before changing your medication, diet, or exercise routine.
References
- American Thyroid Association – thyroid.org – Clinical data regarding the impact of hypothyroidism on Basal Metabolic Rate (BMR) and energy expenditure.
- Journal of Clinical Endocrinology & Metabolism – “The Role of T3 in Human Metabolism” – Research study detailing the metabolic differences between T4-only and T3/T4 combination therapies.
- Mayo Clinic – mayoclinic.org – Overview of Hashimoto’s Autoimmune Thyroiditis and its systemic inflammatory effects.
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) – Official data on the prevalence of thyroid disorders and their impact on weight management.
- Frontiers in Endocrinology – “The Gut-Thyroid Axis” – Peer-reviewed paper explaining how the microbiome influences thyroid hormone conversion.
- Thyroid Journal – “Reverse T3 and the Stress Response” – Clinical insight into how cortisol and chronic stress create metabolic blocks.
- Endocrine Society – endocrine.org – Guidelines on interpreting TSH, Free T3, and Free T4 lab ranges for optimal patient outcomes.