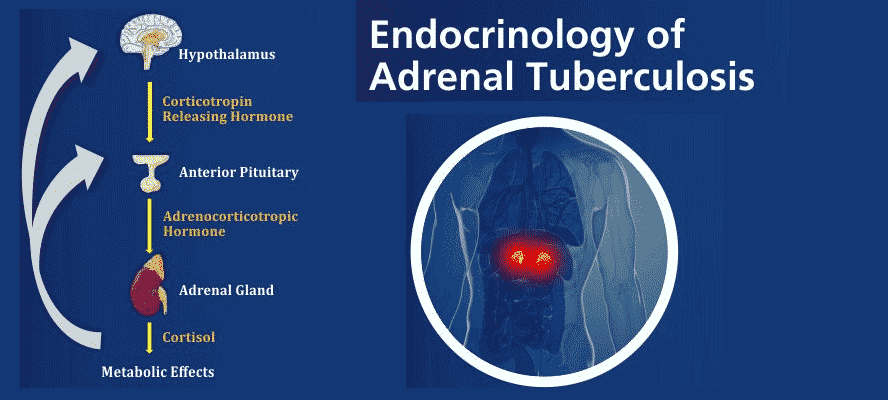
According to the 2019 Global tuberculosis report of World Health Organization (WHO), Tuberculosis (TB) still remains a major public health problem, especially in developing and underdeveloped countries. TB is one of the leading causes of death (alongside HIV) among any other causes by any single pathogen. Although globally the TB epidemic may be on decline, India still harbors the highest TB burden (27%) worldwide. TB is an infectious airborne disease caused by the organism Mycobacterium tuberculosis that generally affects the lungs (pulmonary). Extrapulmonary (any other site excluding lungs) occurrence of TB in the past decade has been on rise accounting for every one in five of the newly diagnosed TB patients and commonly affect sites such as lymph nodes, bone and joints, urogenital tract, and meninges, etc. TB infection of endocrine glands including the hypothalamus, pituitary, thyroid and adrenals have also been reported. TB bacteria once acquired by an individual may remain latent in their body or manifest in active TB disease which can have fatal consequences.