What is Gestational Diabetes?
Gestational diabetes mellitus (GDM) or pregnancy diabetes is a medical condition in which your body fails to produce adequate insulin, which, in turn, leads to a surge in the blood sugar level in pregnancy. Having gestational diabetes does not mean that you had or will have diabetes later in life. However, an unmanaged gestational diabetes range may put you at a higher risk of developing diabetes.
GDM or pregnancy diabetes is of two types – Class A1 GDM and Class A2 GDM. While Class A1 gestational diabetes can be managed with dietary and lifestyle changes, you might need to take insulin medications or injections in case of Class A2 GDM.
Did you know:
- The 2020 GDM rate for mothers under age 20 was approximately 2.5%, substantially lower than the 15.3% rate observed among those aged 40 and above
- The GDM rate in 2020 was 3.7% for underweight women, 4.6% for normal weight women, 7.6% for overweight women, and 12.6% for women with obesity
- Women aged 45 and above face an elevated likelihood of experiencing hyperglycemia during pregnancy. Additionally, women who have previously had gestational diabetes (GDM) are at an escalated risk of developing type 2 diabetes within a five to ten-year timeframe following childbirth.
Gestational Diabetes Symptoms
Some of the key gestational diabetes symptoms during the 24th to 28th week of pregnancy include:
- Extreme fatigue
- Blurred vision
- Excessive thirst
- Frequent urination and other urinary incontinence challenges
- Yeast infections
These signs and symptoms of gestational diabetes mellitus can be easily confused with other health condition symptoms. Thus, a routine GDM screening is highly recommended during the third trimester of pregnancy and up to 3 years after that. Watching out for the signs of gestational diabetes during the third trimester can help you seek on-time diagnosis.
Gestational Diabetes Causes
The symptoms of gestational diabetes depend on the gestational diabetes causes.
Some of the key gestational diabetes mellitus causes include:
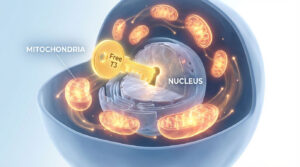
- Excess human placental lactogen – This is a predominant cause of raising the pregnancy blood sugar levels
- Insulin Resistance– This is another key reason for gestational diabetes. Your body fails to produce adequate insulin and as a result, your blood sugar levels go up and your pancreas ends up producing more insulin to keep the blood sugar level in check. Ultimately, due to insulin resistance, you might have higher than normal sugar levels for pregnant women.
Who is at Risk of Developing Gestational Diabetes?
Some of the key risk factors for gestational diabetes include:
- Hypertension
- Family and past history of gestational diabetes mellitus
- Obesity
- Physical inactivity
- High weight gain during pregnancy
- Women with multiple pregnancies and babies
- Women with unexplained pregnancy and delivery complications as well as stillbirths
- Medications, such as glucocorticoids
- PCOS/PCOD
Complications of Gestational Diabetes Mellitus and Impacts on the Body During Pregnancy If Left Untreated
The normal sugar level for pregnant women is 95 mg/dL before a meal, 140 mg/dL 1 hour after a meal and 120 mg/dL 2 hours after a meal. However, if the pregnancy sugar levels are beyond this range, there can be complications both for the mother and the unborn child.
Some of the notable gestational diabetes complications for pregnant women are:
- Hypertension
- Preeclampsia
- Perinatal depression
- Preterm delivery
- Stillbirth
- Emergency C-section
Gestational diabetes complications for the baby include:
- High birth weight
- Birth injuries
- Breathing problems
- Higher risk of diabetes
- Low glucose levels
- Jaundice
Gestational diabetes effect on the baby
Gestational diabetes mellitus when optimally managed might not cause any complications in pregnant women and their babies. However, when left untreated or unmanaged, there can be subsequent gestational diabetes effects on the baby. The baby will be at a higher risk of developing type 2 diabetes later in its life.
Gestational Diabetes Diagnosis
On-time gestational diabetes diagnosis is crucial in keeping both the pregnant woman and her unborn baby safe and healthy.
Some of the key gestational diabetes tests include:
- Routine blood glucose screening
- Glucose challenge test – A at-home blood test to determine sugar levels in pregnancy one hour after the pregnant woman consumes a glass of concentrated glucose solution prepared with 50 grams of glucose dissolved in 250 to 300 ml of water.
- 1-step test – The pregnant woman undergoes a 2-hour 75-g oral glucose tolerance test. The result is deemed abnormal if the sugar level during fasting is beyond 95 mg/dL, 140 mg/dL after the 1 hour mark and 120 mg/dL after the 2-hour mark.
- 2-step test – A 100 gram 3-hour oral glucose tolerance test to identify signs of gestational diabetes during the third trimester.
Management & Treatment of Gestational Diabetes Mellitus
Ensuring the pregnant woman receives the appropriate gestational diabetes treatment is crucial to keep the mother and baby safe and healthy. If you are wondering how to control sugar during pregnancy, you can opt for medical interventions or the management of gestational diabetes mellitus through lifestyle and dietary changes.
Medical Treatment
If you are wondering how to control gestational diabetes during the last trimester of pregnancy, you can either opt for insulin medications or injections as recommended by your healthcare provider.
Home remedies and lifestyle strategies
Some of the key lifestyle changes that can be administered at home to prevent pregnancy diabetes include:
- Diet rich in health-promoting carbohydrates, proteins and fats
- Exercising to maintain physical fitness throughout the pregnancy
- Keeping stress levels in check
Prevention of Pregnancy Diabetes
All women are not susceptible to developing high sugar in pregnancy and it can be certainly prevented through appropriate measures.
Preventing gestational diabetes includes:
- Restricting the use of too much carbohydrates, especially the simple ones
- Avoiding junk and street food
- Having a healthy lifestyle, diet and a sustainable exercise regimen
- Keeping stress levels in check
Gestational diabetes diet
An expert-recommended gestational diabetes diet includes:
- Plenty of whole fruits and vegetables
- Lean proteins and healthy fats – in moderate levels
- Moderate amount of whole grains
- Avoid food rich in sugar, salt and fat content
A Note From HealthcareOnTime
Gestational diabetes can pose significant challenges for pregnant women and their babies. Recognising the high sugar symptoms can help them seek on-time medical treatments and appropriate lifestyle interventions. Opt for periodic blood sugar screening, stay informed and protect your little bundle of joy.
Additionally, for your convenience, consider exploring HealthcareOnTime services that provide sugar test at home. We offer two packages: the Diabetes Test – Basic (covering 69 parameters) and the Diabetes Test – Advance (covering 105 parameters). This option allows you to monitor your health in a more comfortable and stress-free environment, helping you take proactive steps towards a healthier pregnancy.
Disclaimer: The information listed here is strictly for educational purposes and is not intended to offer personal medical advice. Do consult your physician for any questions you may have regarding a medical condition. It’s not advised to disregard professional medical advice or delay in seeking it because of any information listed here. The Nutrition Source does not recommend or endorse any products
Sources
Ref Links: